FAQs
Choose the topic you want to read more about:
- All
- Blepharoplasty
- Brow Lift
- Cataract
- Contoura Vision
- cross-linking
- Diabetic retinopathy
- Dlocked Tear Duct
- Dry Eye
- Entropion
- Epiphora
- General
- Glaucoma
- ICL (Implantable Collamer Lens)
- Keratoconus
- Oculoplasty
- PARS PLANA VITRECTOMY(PPV)
- PRK
- Pterygium
- RETINA
- Strabismus (adult)
- Strabismus (child)
- The Lacrimal Apparatus
What is a cataract?
A cataract forms when the lens of the eye, which is normally clear, becomes foggy and opaque. The affected area may be extremely small or very large and cause a noticeable loss of vision.
Who is affected?
Cataracts mostly affect those aged 60 and over, however, they may also be found in young people and infants.
What causes cataracts?
No one knows what really causes them. However, we do know that the clouding of the lens comes from a chemical modification within the eye which can be related to aging, heredity, trauma or illness. This may be due to advancing age or it may be the result of heredity, an injury or a disease. Excessive exposure to ultraviolet radiation present in sunlight, cigarette smoke or the use of certain medications are also risk factors for the development of cataracts. Cataracts usually develop in both eyes, but often at different rates.
Can cataracts be prevented?
Currently, there is no proven method to prevent cataracts from forming. Wearing sunglasses is a tremendous benefit as they protect your lens from harmful UV rays, which can speed up cataract formation. A diet rich in antioxidants (such as Vitamins A, C, E, Zinc Selenium & Magnesium) is seemingly also beneficial.
What are the signs/symptoms of cataracts?
Cataracts develop without pain or redness, some indications that a cataract may be forming include blurred or hazy vision, the appearance of spots in front of the eyes or the feeling of having a film over the eyes. A temporary improvement in near vision may also occur and increased sensitivity to glare, especially at night, may be experienced.
How are cataracts diagnosed?
A comprehensive eye examination by your optometrist can determine if you have a cataract forming.
How are cataracts treated?
In the early stages of a cataract, where vision is only minimally affected, your optometrist can prescribe new lenses for your glasses to give you the sharpest vision possible. When the cataracts start to interfere with your daily activities and glasses cannot improve this vision, your optometrist will refer you to an eye surgeon who may recommend the surgical removal of the cataracts.
When will I need to have cataracts removed?
Cataracts may develop slowly over many years or they may form rapidly in a matter of months. Some cataracts never progress to the point that they need to be removed. When a change in glasses can no longer provide functional vision, your optometrist will arrange a consultation with a cataract surgeon.
What happens after cataract surgery?
Intraocular lens implants, inserted in your eye at the time of surgery, serve as a “new lens” and sometimes give you good distance vision without glasses. Your near vision will still be blurred. Your Optometrist will prescribe new lenses for your glasses about 4 weeks after surgery to maximize your distance and near vision.
How long does cataract surgery take?
Cataract surgery is performed in a surgical facility and typically takes about 15 – 20 minutes. Your stay at the facility is usually about two hours. You should arrange for someone to drive to and from the facility.
Once surgery is completed, more drops are applied and a protective plastic shield is placed over the eye.
Once home you should rest and avoid strenuous activities.
Is cataract surgery painful?
Cataract surgery is done with anesthetic eyedrops and mild intravenous sedation. There may an occasional sensation of mild pressure but no pain. Some irritation and tearing are to be expected for a few hours after the surgery.
What is the likelihood of complications from cataract surgery?
Sight threatening complications such as serious infection and bleeding are rare (1/1000). Most complications are otherwise minor and transient such as prolonged inflammation, droopy eyelids, elevated intraocular pressure, and retinal swelling.
Retinal detachment can occur after cataract surgery. Very high myopia (nearsightedness) carries an increased risk for retinal detachment.
What smart IOLs for cataract I could use?
We currently offer several advanced technology IOLs, including:
- Monofocal and advanced monofocal (IQ).
- Toric lenses (for astigmatism correction)
- Multifocal lenses and Toric multifocal.
- Extended Depth of Focus Lenses and Toric EDOF.
You need to discuss all above mentioned with your cataract doctor – surgeon- to advice you according to your examination and results.
How does cataract surgery work, and why do you need intraocular lenses afterwards?
During cataract surgery, your natural clouded lens is removed. The lens is then replaced with a clear artificial lens — an intraocular lens — in order for the eye to see its best.
Once an IOL is placed in your eye, it can’t be changed without additional surgery.
What types of intraocular lenses (IOLs) are available?
As you prepare for cataract surgery, you’ll discuss IOL options with your eye surgeon. Several different types of IOLs are available.
What is a premium IOL?
Premium IOLs are designed to offer some freedom from glasses after cataract surgery.
They use advanced technology to correct for eye irregularities and help you focus better up close.
There are several different types of premium IOLs
Premium IOL usually is your choice to facilitate your vision capabilities for all distances ( near, intermediate, far and astigmatism)
What is the difference between the optometrist, ophthalmologist and optician?
The optometrist is the eye exam and eye disease specialist who may also take part in the selling of frames and lenses.
The ophthalmologist performs surgery, treats diseases of the eye and performs eye exams.
The optician can write the optometrist or ophthalmologist’s prescriptions as well as sell frames and lenses.
When should I go for an eye exam?
Generally, recommends visiting your ophthalmologist yearly, unless otherwise stated by your optometrist.
Consult your ophthalmologist as soon as you experience any unusual symptoms that may concern you (blurred vision, headaches, burning eyes, etc.). Some eye diseases are symptomless which is why it is so important to visit your ophthalmologist regularly.
At what age should a child have their first eye exam?
We suggest the first visit by the age of 1, the second at around 2 ½ and annually thereafter. Eyes can be tested as soon as a child is born.
It is important for a child to have an eye exam before starting school in order to ensure there are no vision problems which could affect their learning. A child may also be seen earlier if a parent feels their child squints or has trouble seeing everyday objects.
My child does not know their alphabet and cannot yet read. Can he/she still have an eye exam?
Yes. Optometrists can adapt their exam to children. Images replace letters in order to assess acuity.
How do I choose the right glasses?
Glasses are made up of two parts; frames and lenses. Each must be carefully selected in order to offer you the most satisfaction. Following a complete eye exam, your optometrist and specialized staff can assist you in choosing the frames and lenses best suited to your needs.
The type of corrective lenses you choose are crucial. Before even selecting frames, you must consider the type of lens they must support. The thickness and weight of the lenses are important criteria to consider when choosing frames. Recent technological innovations have led to the development of thinner and lighter lenses, allowing you to select from a wider variety of frames.
Specialized coatings can enhance the performance of your lenses. Scratch resistance improves durability and anti-reflective coating improves visual comfort by reducing eye fatigue caused by light being reflected off the lenses. Anti-reflective coating also enhances your appearance by eliminating glare.
Lastly, in order to choose the right glasses, you must take into consideration what you will be using them for.
Do you work in front of a computer all day? Are you into sports? Are you crafty? Do you read or sew a lot? Are you an outdoors-in-the-sun type or an indoors type of person? Do you live a very active social life and worry about what others think of your appearance? Do you follow trends, enjoy changing your look, your hairstyle, your fashion style? There are so many questions you can ask yourself in order to help guide you in choosing the right glasses.
Selecting several frames to suit your various looks and activities may be a great solution since eye wear is part of your style and fashion.
What are eye floaters?
Eye floaters appear as black or grey specs, strings or cobwebs that shift around when you move your eyes and appear to dart away when you try to look at them directly.
Eye floaters are caused by changes that occur as the jelly-like substance (vitreous) inside the eye becomes more liquid. Microscopic fibers within the vitreous tend to clump and cast tiny shadows on your retina, which appear to you as floaters. Eye floaters are caused for various reasons, some more serious than others.
Are eye floaters serious?
Many people have eye floaters. Floaters that have been present for years and show little or no change are not usually serious. Sudden change in the floaters may be more serious.
Anyone with floaters should be examined by an optometrist promptly. An examination of the retina with dilated pupils is essential to see the back of the eye.
What is the the ophthalmologist looking for if I have floaters?
You optometrist will look into your eyes for an illness or damage to the vitreous or retina. Sudden floaters or flashes in the eye are often caused by a separation of the vitreous and the retina. In about 10% of cases, when this occurs the retina may have ripped of detached itself. In most cases, the retina is not ripped and your ophthalmologist will re-examine your eye at a later date.
What can be done to treat eye floaters?
In most cases, floaters gradually decrease weeks or months later and oftentimes do not completely disappear. Most people learn to ignore them. Eye floaters, like flashes, may disappear even if a rip or detachment of the retina has occurred. Even if the floaters appear to have disappeared, you should be examined by an optometrist.
Your optometrist will discuss treatment options if you have a retinal rip or detachment.
What is colour blindness?
Colour blindness occurs when the ability to differentiate colours and shades is decreased. The term colour blind is often misused. Very few people are actually completely incapable of differentiating colours. Colour vision deficiency is more common in men than in women.
What causes it?
Colour blindness is usually hereditary, but may also stem from illness, trauma or a side-effect of certain medications. Colour blindness occurs when a fault occurs in the development of one or more of the three sets of colour sensing cones in the eye.
What types are there?
There are three types: two affect the red-green and the other, blue-yellow. Red-green colour deficiency is far from being the most common and reflects an inability to differentiate certain shades of red and green. Problems associated with seeing blue-yellow are very rare and reflects an inability to distinguish certain shades of blue and yellow. In very few cases, the inability to perceive colours is so severe that no colours are differentiated. In such cases, the person only sees their world in shades of black, white and grey.
How is colour blindness detected?
Those affected are not usually aware that they are. The simply assume everyone sees this way. For this reason, a comprehensive eye exam is recommended including a colour vision test. The test mainly involves the patient looking at a series of coloured images. A person with normal colour vision will be able to distinguish the shapes in these images.
When should one undergo an Ishihara colour test?
All children should undergo the test by age five. It is important to detect this problem early, as teaching materials in the early years of school involve a good deal of colours. Furthermore, colour blindness could affect one’s career path. Careers such as pilot, electrician, military, police officer and many others require the ability to differentiate colours.
Is colour blindness curable?
Unfortunately, there is still no known cure. However, those affected by colour blindness can compensate by learning to recognize the brightness and position of traffic lights as opposed to their colour for example. Sometimes the ability to differentiate colours can be increased with the help of specialized filters. For example, a red coloured contact lens can be worn in one eye in order to help the patient.
What is a standard IOL?
Standard IOLs are included in the cost of cataract surgery with most medical insurance plans. They are high quality and come in different strengths. Your surgeon will work with you to determine what strength you need.
These lenses are monofocal (also called single-focus) IOLs. They give the sharpest focus at one particular distance — usually a far distance that is helpful for driving. When you want to see up close for reading, or at a middle range for using a computer, you’ll need to wear glasses.
People with astigmatism are likely to need glasses all the time after cataract surgery if they choose standard IOLs.
What is Toric IOLs?
Toric IOLs are single-focus lenses designed for people who have astigmatism.
What is Accommodating IOLs
Accommodating IOLs use your eyes’ own muscles to adjust their focusing power and allow you to see clearly at closer distances.
While these lenses often work well at first, they can sometimes become less effective over time and have been linked to other problems — like tilting or clouding — that could require additional procedures.
What is Multifocal IOLs
Multifocal IOLs contain more than one focusing power within each lens (similar to bifocal glasses but without any line or distortion).
They are designed to help you focus on the far distance, at middle range (for using a computer screen), and up close (for reading) without needing any glasses.
Multifocal IOLs work well in daylight. In the dark, they can make you see halos around lights. This can cause glare and interfere with night vision.
What is Extended depth of focus IOLs
Extended depth of focus (EDOF) IOLs are similar to multifocal IOL but with less focusing power — and fewer side effects. Glare and halos aren’t as big of a problem with EDOF lenses, but their focusing power isn’t as strong, either. In addition to giving you good distance vision, they can help you focus at a middle distance (to see a computer screen), but you’ll still need glasses for reading.
Why choose a premium IOL?
Premium IOLs offer the possibility of freedom from glasses, but they are more expensive and come with a higher risk of side effects.
People choose premium IOLs when they:
- Don’t have other eye problems
- Don’t mind the extra out-of-pocket cost
- Strongly dislike wearing glasses
What is choosing between standard and premium IOLs for cataract surgery?
You’ll want to work closely with your eye surgeon to select your IOLs. There are many factors to consider.
Why choose a standard IOL?
Standard IOLs are less expensive, reliable, and don’t come with many side effects — but most people will still need to wear glasses to see clearly at closer distances.
People choose standard IOLs when they:
- Want the least-expensive option
- Prefer to avoid side effects like glare and halos around lights
- Don’t mind wearing glasses
- Have other eye conditions, like dry eye, glaucomaglaucoma, or macular degeneration, that could interfere with the precise technology used in premium IOLs
Does recovery after cataract surgery depends on type of implemented IOL?
Since standard and premium IOLs are implanted in the same way, the recovery from cataract surgery is the same no matter what type of IOL you have chosen.
How do you know if your IOL is working correctly?
Once your eye has healed from cataract surgery, you’ll begin to use your new lens. You’ll figure out how much glasses can help you focus on objects near and far. No matter what type of lens you’ve selected, it could take some time for you to adjust to the change.
It’s important to remember that even with the most advanced, premium IOLs, many people still need to use glasses to see their sharpest — especially at very close distances.
What I should consider as bottom line?
When you have cataract surgery you will need to choose an IOL. Standard IOLs are high quality and covered by insurance. Premium IOLs can make you less reliant on glasses but come at an additional, out-of-pocket cost.
Will lens implant surgery cause glare or night vision problems?
Night vision after cataract surgery is a common concern. Unwanted images can occur with all implants. These can take the form of glare or starburst. One should expect halos with multifocal implants. Not infrequently, patients observe a shadow in the outer field of their vision after cataract surgery which typically fades over time. Your tolerance to halos will influence your decision about multifocal lenses and will be discussed at your preoperative consultation.
What activities can I do after cataract surgery?
You can resume most of your activities within 3 to 5 days after surgery. Heavy lifting and straining are to be avoided for few days. A protective plastic shield is advised at night for three days to prevent inadvertent eye rubbing while asleep. Makeup should be avoided for 5 days. Swimming and hot tubs are not allowed for 2 weeks.
Consult your doctor about specific activities if you are unsure regarding safety.
How often do I need my eyes checked after cataract surgery?
You will be checked the day after surgery. Depending on your particular case, you will be seen one to three weeks later and again three to six months after that. Annual eye exams are recommended.
Will I have to have cataract surgery again in the future?
Lens implants are typically not subject to deterioration and should last a lifetime.
Some patients will experience a subsequent clouding of the membrane which holds the lens, called the capsule. This clouding will cause blurred vision and is easily fixed with a non invasive laser (YAG laser) beam that creates an opening in the membrane allowing restoration of a clear path for light. This procedure is called a capsulotomy.
What is glaucoma?
Glaucoma is an eye disease in which it is thought the internal pressure of the eye rises to a point that the optic nerve is damaged. The pressure that builds up is due to a problem in the production, flow or drainage of fluid normally produced in the eye. Glaucoma is one of the leading causes of permanent vision loss in Canada.
What causes glaucoma?
The exact cause of glaucoma is not known. For some reason, there is an overproduction of fluid and/or the passages that normally allow fluid within your eye to drain out become clogged or blocked. This results in fluid building up within your eye and increasing pressure on the optic nerve. The nerve fibers and blood vessels in the optic nerve can easily be damaged by this pressure. An injury, infection or tumor in or around the eye can also cause the pressure to rise.
Who is affected by glaucoma?
Glaucoma most frequently occurs in individuals over the age of 40 and there is a hereditary tendency for the development of the disease in some families. Primary open-angle glaucoma causes damage at an earlier age and leads to vision loss at a much greater rate. There is also a greater risk of developing glaucoma when you have diabetes, high blood pressure and eye injuries. Regular optometric examinations are important for all ages to assess your risk for glaucoma.
What are the different types of glaucoma?
There are different types of glaucoma, but they can be broadly divided into two groups: chronic open-angle and closed-angle.
- Chronic open-angle glaucoma: is the most common form of glaucoma. The drainage angle of the eye becomes less efficient over time, and pressure within the eye gradually increases, possibly resulting in damage to the optic nerve. In some patients, the optic nerve becomes sensitive even to normal eye pressure and is at risk for damage. Treatment is necessary to prevent further vision loss. Risk of developing chronic open-angle glaucoma increases with age.
- Open-angle glaucoma: typically has no symptoms in its early stages, and vision remains normal. As the optic nerve becomes more damaged, blank spots develop in the field of vision. You may not notice these blank spots during day-to-day activity until the optic nerve is significantly damaged and these spots become large.
- Closed-angle glaucoma: occurs in certain eyes when the iris is very close to the drainage angle. These eyes are often small and farsighted, and the iris could be sucked into the drain and block it completely. Since the fluid cannot exit the eye, pressure can build up rapidly, resulting in acute closed-angle attack.
Symptoms may include:
- Blurred vision
- Severe pain
- Headaches
- Rainbow halos around lights
- Nausea
- Vomiting
Will glaucoma cause blindness?
The optic nerve at the back of the eye, carries visual information to the brain. As the fivers that make up the optic nerve are damaged, the amount and quality of information sent to the brain decreases and a loss of vision occurs.
How can I tell if I have glaucoma?
Primary open-angle glaucoma often develops painlessly and gradually. There are no early warning signs. It can gradually diminish your vision without you knowing it. Acute angle-closure glaucoma may have symptoms such as nausea, eye pain, red eyes, blurred vision and haloes around lights.
A comprehensive ocular health examination is often the only way to detect glaucoma. Your visual acuity can remain a sharp 20/20 in the beginning stages of this condition. Your optometrist will include in your examination a simple and painless procedure called tonometry, which measures the internal pressure of your eye. Your optometrist will also look into your eye to observe the health of the optic nerve.
Who is at risk for glaucoma?
Your ophthalmologist considers different kinds of information to determine your risk for developing the disease. The most important risk factors include:
- Age
- Elevated intraocular pressure
- Family history of glaucoma
- African or Spanish ancestry
- Farsightedness (closed-angle) or nearsightedness (open–angle)
- Past eye injuries
- Thinner central corneal thickness
- Systemic health problems including diabetes, migraine headaches, and poor circulation
Your ophthalmologist will weigh all these factors before deciding whether you need treatment or monitoring as a glaucoma suspect, which means your risk of developing glaucoma is higher than normal, and you need to be followed closely to detect early signs of glaucoma.
How is glaucoma detected?
Regular eye examinations by your eye doctor are the best way to detect glaucoma. A glaucoma screening that only checks pressure is insufficient to determine if you have glaucoma.
During a glaucoma evaluation, the ophthalmologist will measure your intraocular pressure (tonometry), inspect the drainage of your eye (gonioscopy), evaluate any presence of optic nerve damage (ophthalmoscopy), and test the field of vision of each eye (visual field testing of perimetry). Photography of the optic nerve or computerized imaging may be recommended. These tests may need to be repeated on a regular basis to monitor any changes in your condition.
How is glaucoma treated?
As a rule, damage caused by glaucoma cannot be reversed. Eye drops, laser surgery, and surgery (in the operating room) are used to help prevent further damage. In some cases, oral medications may also be prescribed. With any type of glaucoma, periodic examinations are important to prevent vision loss. Glaucoma can progress without your knowledge, hence the need for routine follow-up visits to check the progression of the disease and adjust therapy as needed.
Medication
Glaucoma is usually controlled with medicated eye drops each day. The drops lower eye pressure by reducing aqueous production or increasing outflow through the drainage angle or other tissue. Never change or stop taking medication without consulting your ophthalmologist. Glaucoma medications can preserve vision but may also produce side effects.
Notify your ophthalmologist if you think you are experiencing side effects, including:
- A stinging or itching sensation
- Blurred vision
- Changes in breathing (especially with asthma or emphysema)
- Changes in energy level
- Changes in eye color
- Changes in pulse and heartbeat
- Changes in sense of taste
- Dry mouth
- Headaches
- Red eyes or redness of the skin surrounding the eyes
All medications can have side effects or possible interaction with other medicines. It is important to make a list of all medications you regularly take and share it with every doctor you see.
Laser surgery
Laser surgery treatment may be recommended for different types of glaucoma. In open-angle glaucoma, the drain itself is treated. The laser is used to modify the drain (trabeculoplasty) to help control eye pressure. In closed-angle glaucoma, the laser creates a hole in the iris (iridotomy) to improve the flow of aqueous fluid to the drain.
Microsurgery
When surgery in the operating room is needed to treat glaucoma, your ophthalmologist uses fine, microsurgical instruments to create a new drainage channel for the aqueous fluid to leave the eye. Surgery is recommended if your ophthalmologist feels it is necessary to prevent further damage to the optic nerve.
What is PRK Eye Surgery?
Photorefractive keratectomy (PRK) eye surgery is a type of refractive eye surgery that is typically used to treat mild forms of nearsightedness (myopia), farsightedness (hyperopia), and blurry vision (astigmatism). PRK is similar to LASIK eye surgery in that it improves the patient’s vision long-term, potentially eliminating the need for corrective glasses, reading glasses, and contact lenses altogether. However, PRK is generally recommended for patients who have mild blurred vision, dry eyes, or thin corneas.
Who Is a Candidate for PRK Eye Surgery?
PRK eye surgery is recommended for those with thin corneas due to its more precise treatment approach. It does not disrupt as much corneal tissue as LASIK surgery, so it is suited for those with less corneal tissue to begin with. In addition, PRK eye surgery has a short recovery period and a low risk of vision-threatening complications.
Does PRK hurt?
Prior to the PRK procedure, your doctor applies numbing eye drops to block the feeling of pain. While every person has their own unique threshold for discomfort, most patients do not report that the process is painful. The PRK recovery process may bring you temporary discomfort as the epithelial cells regenerate on your eye. These discomforts can include pain, throbbing, a foreign substance feeling, etc. This can be managed with pain medications outlined by your doctor.
How to Prepare for PRK Eye Surgery?
Preparing for PRK eye surgery is an important part of ensuring a successful procedure and minimizing any risks.
First, it’s important to visit your ophthalmologist for an eye exam to ensure that you are a good candidate for the procedure. Prior to this exam, you should stop wearing rigid contact lenses for at least one week to ensure your eyes can be properly evaluated before surgery. If you wear soft contact lenses, stop them at least three days before this appointment.
Once your surgery is scheduled, make sure to ask someone to drive you home on the day of the procedure since your vision will be blurry immediately after the surgery.
Lastly, be sure to follow your doctor’s instructions on post-operative care, such as using eye drops and avoiding activities that could cause further harm to your eyes.
What are the requirements for PRK?
There are several conditions that must be met to be considered for PRK:
- 18 years or older
- Stable vision prescription for at least one year
- Free of eye disease or other interfering vision conditions
- Proper corneal thickness
- Good overall health
- Realistic expectations
- Full understanding of the potential risks
The only way to know if you meet these requirements is by having a comprehensive PRK Consultation with us. It’s free and will let you know for sure if this is a safe option for vision correction for you.
What to Expect During PRK Eye Surgery?
During your PRK procedure, you’ll be asked to lie down on a table. Your board-certified doctor will provide you with medicated eye drops to numb your eyes, ensuring you remain comfortable throughout your treatment process. An instrument will be used to hold your eyelids open while the laser procedure is performed.
Next, your doctor will use an alcohol solution, brush, or small blade to remove the outermost portion of your cornea, called the epithelium. This gives your doctor access to the cornea and using advanced laser technology, your provider will reshape your cornea. You’ll likely be asked to focus on a point of light throughout your procedure, and your vision may dim. This is normal and is no reason for concern. Your entire procedure should take 10 to 15 minutes to complete.
How long does PRK take?
The full PRK procedure takes 10 minutes, from the time you enter our surgical suite until you go into the recovery area. The excimer laser treatment where we reshape your cornea takes about 5 minutes!
How long will I need to be off work?
Because your eyes need time to recover an intact outer layer on the cornea, expect to take 5-7 days off from work to recover from PRK . Your best vision results will probably take longer to achieve, but most patients are able to return to non-strenuous activities after 1-2 weeks. It is important to keep your follow-up visits so your doctor can monitor your progress
Recovering from PRK Eye Surgery
PRK recovery time is minimal, lasting just a few weeks to a month. Immediately following your PRK procedure, your eyes may feel slightly uncomfortable. Itching, burning, and a gritty sensation a few days after surgery is normal; however, it’s important you DO NOT rub your eyes at any point. Your Ophthalmologist will give you medicated eye drops to use several times throughout the day and protective eyewear to ensure you stay comfortable throughout your recovery period.
It’s important to note that your vision may take some time to fully restore. Our patients often find their vision is slightly blurry for the first few weeks following their PRK procedure surgery. However, vision should improve greatly by one month after the procedure. We also ask that patients avoid using cosmetics around the eyes for several weeks following surgery to ensure the eyes are not irritated during the healing process.
Will I ever need glasses after PRK?
Your vision is constantly changing. While PRK is performed to correct a refractive error, other vision conditions can develop that may require you to need glasses in the future. Most people over age 40 develop a condition called presbyopia. This is a gradual stiffening of the eye lenses that makes it difficult to focus on things up close like reading material. Even if you had a successful PRK procedure, you may need over-the-counter reading glasses as you grow older. There are also different surgical methods to correct presbyopia. If you are experiencing this condition and are frustrated with reading glasses, contact us to learn about your treatment options.
Benefits of PRK Eye Surgery
There are many benefits of receiving PRK eye surgery with the doctors at The Surgical Eye Center, including:
- Minimally invasive procedure (Safest)
- Short procedure time.
- Restores vision for patients with nearsightedness, farsightedness, and astigmatism
- Eliminates the need for glasses, reading glasses, or contacts for most activities
- patients gain 20/20 vision
- Long-lasting, potentially permanent results
- High-quality, personalized care (customized procedure)
- Consultant of Surgical Eye center will be carrying out your procedure
- Cost-effective
What Is Contoura Vision Eye Surgery?
In the healthcare industry, advanced technologies are developed to make patients’ lives easier and healthier, Many patients cannot profit from the technology available in the business. Thus technological improvements are essential in this sector.
Such individuals either have a completely new disease or have a condition that has progressed to the point where it can no longer be treated with the present system of drugs and procedures, These improvements are not limited to spectacles removal surgery. Scientists are working hard to develop surgical treatments with the fewest possible risks and the most excellent possible outcomes.
Contoura Vision surgery, commonly called Topography-guided LASIK surgery, is one such sophisticated procedure, This procedure is a more sophisticated type of LASIK that offers more benefits to individuals considering spectacle removal surgery.
Not only is this procedure successful in general people, but it also produces good outcomes in patients who were previously ineligible for LASIK surgery owing to corneal abnormalities, The USFDA has given its approval for the technology to be used to remove the specifications.
What is the Contoura Vision Eye Surgery History?
The practice of wearing spectacles to correct vision dates back to the 13th century, Contact lenses made from hand-blown glass were available in Switzerland in the 1800s, These were the non-invasive ways for enhancing visual clarity and correcting eyesight.
These gadgets, on the other hand, inflict discomfort to the patient and need thorough treatment, As a result, intrusive eyesight correction procedures are being introduced, Radial keratotomy, which involves making an incision on the cornea with a diamond knife and altering its curvature, was invented by a Russian eye specialist.
Astigmatism is still managed with this method, In the 1990s, the USFDA authorized a more powerful technique for eyesight correction, The procedure is called photorefractive keratome, and it provides long-term vision correction, LASIK combines the benefits of each preceding procedure while eliminating their drawbacks, resulting in far greater patient satisfaction.
These procedures have proven very effective and are still regarded as the gold standard in vision corrective surgery, In 1999, a personalized LASIK treatment based on wavefront analysis became available.
Contoura was the name of the method, which provided 22000 points on the cornea, Conventional LASIK maps just 200 locations on the cornea compared to Contoura.
What are Contoura Vision’s Benefits?
- Removal procedures
FDA-approved in the United States, Contoura Vision has been certified by the US Food and Drug Administration, claiming the most significant level of safety in the corrective refractive errors.
- What are the advantages of Contoura Vision?
• The benefits are numerous:
• An even higher degree of precision for vision correction.
• Results that lead to the smoothest possible cornea.
• Reduction in subtle post-operative symptoms from standard wavefront-optimized LASIK such as halos, glare, or difficulty driving at night.
- Removal of corneal irregularities
Contoura Vision can map and erase corneal abnormalities by identifying 22,000 distinct elevation points on the cornea with Surgical Eye centers, This is capable of creating an optically flawless smooth corneal surface, significantly improving visual sharpness and quality.
- Treatment of the visual Axis
Contoura Vision works with the visual axis, which is the eye’s natural seeing axis, LASIK is a treatment that focus on the pupillary axis, this therapy on the Visual Axis improves eyesight quality even further.
What is WaveLight LASIK?
WaveLight® LASIK technology uses a laser beam to reshape the surface of the eye, making it effective at focusing light and ultimately leading to better vision.
What is the difference between Contoura and SMILE?
We have discussed tiny incision lenticular extraction (SMILE) as an alternative to LASIK, with promising findings that show SMILE might be even better (SMILE vs. LASIK).
However, research from high-end treatment outcomes suggests that topography-guided LASIK might be even more effective, Simply put, it is the most sophisticated LASIK option and the most advanced vision correction technique, Which isn’t to suggest that conventional LASIK and Wavefront-guided LASIK aren’t effective in improving vision, They continue to produce good outcomes with little danger of adverse side effects.
Topography-guided LASIK, on the other hand, maybe even superior, Contoura also offers the added benefit of decreasing the risk of light sensitivity, glare, and halos following treatment, according to FDA documents.
What are the findings of the Contoura Vision studies?
The USFDA has authorized Contoura vision surgery for vision correction, the permission is given after a thorough examination of the applicant’s or innovator’s extensive research, Patients who had Contoura vision surgery had greater than 100 percent vision, according to research, In the three-month follow-up, it was also discovered that the Contoura vision surgery was significantly superior to SMILE.
Who is a Good Candidate for Contoura Vision Surgery?
Not all individuals with visual issues are candidates for topography-guided LASIK, The ophthalmologists would perform a thorough examination of the patient’s eyes to see if the Contoura vision surgery will help them enhance visual clarity or correct refractive errors.
The following patients are not candidates for Contoura vision surgery, such as:
- Patients under the age of 18 years old who have visual problems
- The patient who has an immune deficiency illness
- Patients suffering from vascular disease
- Patients who have myopia of more than 9.00 D
- Patients have a large nose and brow that prevents them from seeing themselves in the mirror
- The doctor will determine other requirements on a case-by-case basis.
Why Choose LASIK Contoura Vision?
There are many benefits to choosing LASIK Contoura Vision over other forms of laser vision correction. Here are a few:
- Permanent removal of spectacles /contact lens
- Personalized treatment: The Contoura Vision system creates a customized treatment plan based on your unique eye shape and vision needs, ensuring that your vision is corrected as precisely as possible.
- Enhanced safety: The Contoura Vision system is designed to minimize the risk of complications and ensure that the procedure is as safe as possible.
- Quick recovery: Most patients are able to return to work and other activities within a day after the procedure. It is a single-day walk in – walk out procedure
- Corrects visual axis
- Removes irregularities in the cornea
- No pain, no cut, no stitches, no hospitalization
- Unmatched by any LASIK or SMILE procedure
Sharper visual results as compared to LASIK and SMILE
Contoura Vision – Real Personalization
Contoura vision provides a method that is absolutely unique to your eyes. The cornea’s surface is not totally smooth and has some minute imperfections, and Contoura Vision is able to map these abnormalities using 22,000 unique data points and then correct these flaws, providing an optically flawless surface of the cornea, giving you sharpness unmatched by any LASIK or SMILE laser eye surgery. This is done through a device called a corneal topographer which creates a 3D map of the surface of your eye. The topolyzer identifies corneal abnormalities, improves eyesight sharpness, and transforms the cornea into an optically flawless surface.
Contoura Vision – A real satisfaction
In your eyes, there are two types of axes:
- Pupillary Axis: A line that runs through the centre of the eye
- Visual Axis: A line padding along the eye’s line of sight
The angle between these axes is 5 degrees.
While LASIK and SMILE laser operations target the pupillary axis, Contoura Vision treatment treats the visual axis, offering far finer visual outcomes than LASIK and SMILE.
What Is Keratoconus ?
is a progressive eye disease that turns your normally round cornea into a bulging cone shape. The cornea is an important part of the eye that is responsible for two main things:
- Bending and focusing light so you can see, similar to how a camera uses light to capture photographs
- Protecting your eyes from dirt, germs and harmful UV rays
In people with Keratoconus, the light bends in unusual ways depending on what part of the bulging cornea the light passes through.
What Are the Symptoms of Keratoconus?
Keratoconus has many symptoms, including…
- Blurry and distorted vision
- Double vision with one eye closed
- Triple “ghost” images
- Night time halos
- Streaks when viewing bright lights
Sensitivity to light, and frequent headaches.
How Can Keratoconus Affect My Life?
Keratoconus affects your vision which can degrade your quality of life. Individuals with this disease may find it hard to work, read, watch TV, and drive. It can also stress, lower your confidence, make you unable to enjoy those important moments in life, reduce your ability to take part in recreational sports, and affect your personality.
How Common Is Keratoconus?
Keratoconus is a lot more common than people think. In the past, it was predicted that 1 in 2,000 people had it, while today that number has drastically increased to 1 in 400. The reason for this increase is that more people are properly diagnosed due to advances in technology, and awareness.
What Causes Keratoconus?
There is no firm consensus in the medical community about the causes of Keratoconus. However, we do know that it develops when the collagen protein fibers in the eye weaken. When collagen in the eye weakens, it can cause the cornea to lose its shape. (Think back to your days on a playground when a rubber ball became lopsided with a bulge on one side.)
One cause of this weakness could be due to free radicals in your eyes. Every day, your corneas produce harmful by-products known as free radicals. Antioxidants in your eyes typically get rid of these free radicals, but individuals with Keratoconus don’t produce enough antioxidants to fight off the free radicals. As collagen levels decrease, the corneas lose their strength and start to bulge.
The weakness can also be caused by frequent rubbing of the eyes. There may be a genetic component as well, since those with KC in their family are more likely to also have the condition.
Are There Multiple Forms of Keratoconus?
Keratoconus comes in a variety of forms. Depending on your symptoms, you may be experiencing one of the following forms of this disease:
- Forme fruste Keratoconus is a mild form and a precursor of the disease. It is a mild form of the condition that usually causes few issues.
- Nipple cone Keratoconus involves the cornea forming a cone-like shape. Common symptoms include blurry and distorted vision.
- Oval cone Keratoconus is a version where the cornea bulges into an oval shape. The bulging tends to occur at the bottom outer part of the cornea and can make it look as if it is sagging.
- Pellucid Keratoconus is a version of KC with inferior thinning of the cornea from the outside in.
- Globus cone Keratoconus is the most severe form of the disease. It causes an individual’s cornea to thin and bulge into a round shape.
How Is Keratoconus Diagnosed?
There are several methods available for diagnosing Keratoconus. These methods include:
- Eye refraction where an Optometrist uses special equipment to analyze your eyes for vision problems.
- Keratometry which involves your eye doctor focusing a circle of light into your cornea to measure the reflection and check the shape of your cornea.
- Slit-lamp exam involves an eye doctor shining a vertical beam of light on your eye and a microscope to analyze the surface of it. This test assesses the shape of your cornea and can spot other problems too.
- Corneal mapping is a more advanced technique that uses specialized optical coherence tomography and corneal topography to map the shape of your cornea.
- Pachymetry is a test to measure the thickness of the cornea.
What is the Best Keratoconus Treatment?
Scleral contact lens.
Cross linking to fix the modification on cornea.
ICL: Implantable Collamer Lens.
PKP, (Penetrating Kerato-Plasty) in advanced cases.
Does Keratoconus Cause Eye Pain?
Keratoconus doesn’t always cause eye pain. However, its symptoms can cause discomfort and other problems. The most common symptoms of Keratoconus include astigmatism, degrading vision quality, and corneal thinning, bulging, or rounding. Some individuals may experience corneal scarring and find themselves unable to use contact lenses. These individuals may require a corneal transplant to correct this problem.
If you have Keratoconus and experience sudden pain in your eyes, you should consult with your Keratoconus specialist immediately.
Can Keratoconus Go Away On Its Own?
Keratoconus is a lifelong eye disease that does not go away on its own. In severe cases a corneal graft might be needed, but that does not eliminate Keratoconus. Individuals with less severe Kerataconus can reduce its effects using specialized contact lenses (hard, piggyback, hybrid, or scleral). Scleral lenses are a unique type of contact lens that rests on the white part of your eye (the sclera) and does not sit on the cornea.
What Do I Do If I Think I Have Keratoconus?
Contact your ophthalmologist for routine cornea exam.
What is cross-linking?
Cross-linking is a minimally invasive, FDA approved, outpatient procedure that combines the use of prescription eye drops (Riboflavin) and ultra-violet A (UVA) light from the CXL device for the treatment of progressive keratoconus or post-LASIK ectasia. This treatment stabilizes the cornea to prevent further progression.
What are the indications for crosslinking?
Accepted medical indications for corneal cross-linking include the following:
- Individuals with keratoconus, with documented progression of corneal ectasia.
- Children with keratoconus, who are eye rubbers.
Individuals with LASIK-induced corneal ectasia.
What is corneal cross linking used for?
Corneal cross linking is a minimally invasive procedure that uses ultraviolet light and eye drops in order to strengthen the collagen fibers in the cornea. The procedure is used for patients with keratoconus, a condition in which the cornea grows thin and weak.
What can I expect during the procedure?
- After numbing drops are applied, the epithelium (the thin layer on the surface of the cornea) is gently removed.
- Riboflavin Viscous eye drops will be applied to the cornea for at least 30 min.
- Depending on the thickness of your cornea, Riboflavin drops may also be required.
- The cornea is then exposed to UV light for 30 minutes while additional Viscous drops are applied.
- A bandage contact lens is placed on your eye.
What is ultra-violet A (UVA) light?
UVA is one of the three types of invisible light rays given off by the sun (together with ultra-violet B and ultra-violet C) and is the weakest of the three.
Does corneal cross-linking require removal of the epithelium?
Yes, the FDA approved protocol specifies that the epithelium is removed for the procedure. Your doctor will apply topical anesthesia to numb the eye prior to the removal of the epithelium. This process helps to prepare your eye so that the drug can penetrate the tissue of the cornea to have an effective cross-linking procedure.
Am I awake during the procedure?
Yes, typically you will be awake during the treatment. You may be given a medication to help you relax, and numbing anesthetic drops.
How long does the treatment take?
The actual procedure takes about an hour, but you will be at the office for approximately two hours to allow sufficient time for preparation and recovery before you return to the comfort of your own home.
What can I expect after the procedure?
- You should not rub your eyes for the first five days after the procedure.
- You may notice a sensitivity to light and have a foreign body sensation. You may also experience discomfort in the treated eye and sunglasses may help with light.
- If you experience severe pain in the eye or any sudden decrease in vision, you should contact your doctor.
- If your bandage contact lens from the day of treatment falls out or becomes dislodged, you should not replace it and contact your doctor.
Does it hurt?
There is some discomfort during healing but usually not during the treatment. Immediately following treatment, a bandage contact lens is placed on the surface of the eye to protect the newly treated area. After the numbing drops wear off, there is some discomfort, often described as a gritty, burning sensation managed with Tylenol and artificial tears.
Is cross-linking right for me?
Patients who have been diagnosed with progressive keratoconus should ask their doctor whether they may be an appropriate candidate for corneal cross-linking.
When should cross-linking be done?
Patients of any age may be considered as a candidate for corneal crosslinking to treat keratoconus. Patients 14 years old and over can have very good results with this treatment. Making the diagnosis as early as possible is important, and this typically requires corneal topography or tomography.
What to avoid after crosslinking?
For the first week, please avoid more strenuous exercise such as running and aerobics (in case of injury or sweat running into the eyes). recommended to avoid getting water in your eyes until you have been checked at your one-week follow up appointment. For the first month you should also not swim in chlorinated water.
What is Implantable Collamer lens?
Implantable Collamer Lens or ICL is a new intraocular lens that can be implanted into the eye without removing the natural lens. This lens is an excellent choice for patients with short-sightedness (myopia), long-sightedness (hyperopia) and astigmatism. This lens is made from a material called Collamer, a collagen co-polymer that contains a small amount of purified collagen. Since it is stable and biocompatible, the lens is highly safe, soft, flexible and moist. Due to the ICL is implanted through a microscopic incision that requires no stitches, it does not alter the natural shape or health of the cornea. The ICL is a new intraocular lens, therefore there are some frequently asked questions, find out the correct answers here to strengthen confidence before making decision.
What are the differences between the ICL and LASIK?
The ICL or Implantable Collamer Lens is a new intraocular lens that can be implanted into the eye without removing the natural lens. This lens is made from a material called Collamer, a collagen co-polymer that contains a small amount of purified collagen. It is stable and biocompatible and it has been used for many years in the lenses implanted during eye surgery. The lens is small, foldable, soft, flexible and moist. Due to the ICL is implanted through a microscopic incision that requires no stitches, it does not alter the natural shape or health of the cornea. It can remain inside the eye indefinitely. If the vision changes significantly, the lens can be further removed. In addition, lens does not affect corneal curvature and damage cornea tissue. While LASIK surgery corrects vision by reshaping the clear front surface of the eye ( cornea) with an ultra-precise laser. LASIK or Laser-Assisted In Situ Keratomileusis is a surgery that corrects vision by changing the shape of the cornea permanently with an ultra-precise laser. The ICL is an alternative for some patients who are not suitable for LASIK because the cornea is not thick enough to be treated safely with laser eye surgery procedures.
Can patients with mild short-sightedness be treated with the ICL?
Yes. The ICL can be used to treat patients with short-sightedness or myopia, ranging from -0.50 up to -18.00 eyesight. In addition, the lens can be used to treat astigmatism with -0.25 to -6.00 eyesight.
Can colored contact lenses be worn after ICL surgery?
Yes. If the patients do not experience dry eyes, colored contact lenses can be worn regularly 1 month after ICL surgery.
Does ICL surgery hurt?
Anesthetic eye drops are used to numb the eye before surgery begins. Patients will not experience pain during procedure. A small instrument will be placed between eyelids to prevent blinking. The customized lens is folded into a special injector. An ophthalmologist will make a small incision (sized 3-3.2 mm) in the cornea to insert the ICL. After the ICL is inserted inside the eye, the ICL will unfold and be positioned between iris and crystalline lens. The opening then seals on its own, usually without the need for stitches. Patient might feel irritated in the eyes. However, patients can communicate with the ophthalmologist while operating at all times.
Can both eyes be treated with the ICL at the same time?
The ICL can be performed in each eye or both eyes at the same time. However, personal consultant with ophthalmologists is highly needed prior to operation.
If one side of the eyes underwent LASIK while another side was treated by the ICL, does this affect eyesight? Is special care additionally required?
It is highly recommended to have ICL surgery for both eyes. However, if different procedures had applied to each eye, it does not cause any vision-related problems.
Is ICL surgery recommended in the elderly?
In case of elderly patients, if patients do not develop cataract, ICL surgery might be recommended. However, this procedure is suitable for patients aged younger than 45. Patients aged over 45, cataract might be a concern and medical counseling with ophthalmologist is individually required.
What are possible reasons to remove the ICL from the eyes? How is the ICL removed?
his lens is made from a material called Collamer, a collagen co-polymer that contains a small amount of purified collagen. It is small, foldable, soft, flexible and moist. Since it is stable and biocompatible therefore it does not cause any tissue damages. To remove the lens, it is similar to how to implant it at the beginning. Due to advanced age, cataract development is the most common reason to remove the lens. If cataract surgery is needed, the lens must be also removed. Other possible reason, although it is rare, is an increased intraocular pressure in the eyes. Intraocular pressure might temporarily increases after surgery. After medicines that lower pressure in the eyes are taken, if elevated intraocular pressure does not relieve after ICL surgery, the lens might need to be removed
What is the lifespan of the ICL?
Since the lens is biocompatible with tissues, so it can remain inside the eye indefinitely, unless vision changes.
Can I go to gym after ICL surgery?
Because ICL surgery is intraocular surgery, we ask you not to do any vigorous exercise for the first week after surgery. Usually after a week, the eye’s healed nicely and you’re welcome to carry on with your normal sporting activities after a week.
Can I use laptop after ICL surgery?
Reading, computer work, watching television, and flying are all fine to do immediately. You can restart your regular exercise regimen the morning after surgery.
How do you shower after ICL surgery?
When you shower or bath, avoid getting soap/water directly in the operative eye(s) for 5 days after surgery. Avoid bumping or rubbing your eyes the first five days after surgery. Avoid swimming, hot tubs, and water sports for five days after surgery.
An ICL be dislocated?
Dislocation of ICLs after blunt trauma is a rare but important potential sequela of the procedure and can lead to corneal decompensation if there is lens-endothelial touch. All patients who suffer blunt dislocation of ICL should be followed long-term after repositioning for signs of endothelial loss and dysfunction.
Is ICL more risky than LASIK?
A primary difference between ICL surgery and LASIK surgery is that ICL surgery has an increased serious infection risk over LASIK. This is because the surgeon has to go inside the eye to place the ICL, while the LASIK procedure is performed on the cornea without entering the inside of the eye.
What is Pterygium?
Obviously, this is one of (if not the most) the most common questions about pterygium. Pterygium is a growth of fleshy tissue around the conjunctiva. The conjunctiva is the membrane that lines the eye and keeps the surface of your eye moist. This helps protect your eye from dust, debris, and germs.
Pterygium usually forms on the corner of your eye and can extend onto the cornea—the eye’s clear, protective outer layer. When the growth stays within the conjunctiva, it’s called pingueculum. But when it spreads from the conjunctiva to the cornea, it’s known as pterygium.
A pterygium can be of various shapes and colors, such as red, pink, white, gray, yellow, or even colorless. Some pterygium growths can be pretty small, while others can be big enough to cause irritation, blurred vision, and other issues.
What are the Signs and Symptoms of Pterygium?
The signs and symptoms of pterygium include:
- Eye irritation and burning
- Dry eye
- Redness
- Blurred vision (if the growth gets close to the cornea)
- Feeling like you have a foreign object in your eye
- Gritty eyes (scratchy or rough feeling)
- Itchiness
- Yellow spot or bump on the white of the eye
Sometimes, people with pterygium don’t experience symptoms. However, if they do, the symptoms are typically mild.
What Causes Pterygium?
Research shows that the risk factors for pterygium fall under three categories: demographic, environmental, and lifestyle factors.
- Older age: According to research, the risk of developing pterygium increases with age.
- Being male: Men are at greater risk of developing pterygium than women.
- Long-term exposure to sunlight: People who spend a lot of time outdoors are more likely to develop pterygium, especially in sunny climates. Ultraviolet (UV) rays play a key role in causing pterygium. UV radiation induces inflammatory cytokines, which causes excessive blood vessels, cells, and tissue to form.
- Excessive smoking and alcohol consumption: Cigarette smoking can cause inflammatory responses in the cornea, which can contribute to pterygium. Excessive alcohol intake can also increase the risk of pterygium.
- Family history of eye disease: People who have a family history of pterygium may be at higher risk for developing this condition.
- Exposure to certain allergens: Other agents that can increase your risk of pterygium are allergens such as dust, dirt, air pollution, and chemicals.
If you’re a male who smokes and drinks, has a family history of eye disease, is middle-aged, and spends a lot of time outdoors, you’re more likely to develop pterygium. These factors can occur all at once or individually. However, the condition can also occur without these factors.
How Do Ophthalmologists Treat Pterygium?
How your doctor treats your pterygium will depend on the severity and size of the growth. It also depends on where it’s growing within the eye and its effect on the eye.
For example, suppose you have a small pterygium. In that case, it may be best for your doctor to take a conservative approach by prescribing artificial tears or eye drops to fight dryness, irritation, and the feeling that “something is in the eye”.
If the growth is larger and affects your vision, your ophthalmologist may perform pterygium excision surgery to remove the growth. Other reasons your doctor may surgically remove the growth include irritation and cosmetic concerns.
Additionally, the success rate of pterygium excision surgery is relatively high if your doctor removes the growth before it reaches the center of the cornea.
In general, the procedure is simple. You’ll go under local or topic anesthesia. You can receive this treatment on an outpatient basis, which means you’ll be able to go home the same day after the procedure.
After surgical removal of the pterygium, there’s a chance that the growth can come back. However, some research shows that the recurrence rate of pterygium has significantly declined over the past few decades.
How Do You Prevent Pterygium?
While there’s no sure way to prevent pterygium, there are things you can do to lower your risk of developing the condition. This includes:
- Wearing sunglasses to protect your eyes from UV rays
- Wearing a hat to shield your eyes from sunlight, wind, and dust
- Avoiding exposure to environmental irritants such as smoke, dust, wind, and chemical pollutants
Taking these steps can also help if you already have a pterygium and want to minimize symptoms. It can also help prevent recurrence if you’ve had surgery to remove the growth.
What Should I Do If I Think I Have Pterygium?
All in all, pterygium is a relatively harmless condition. However, it takes an expert in ophthalmology to correctly diagnose the condition and suggest the proper treatment. If you suspect that you have pterygium, schedule an appointment with Surgical Eye Center Doctors.
What is the vitrectomy?
Vitrectomy surgery is a surgical procedure that removes the vitreous humor/gel. It is performed for a variety of reasons/conditions. The essence for removing the gel is to eliminate the traction of the gel from the retina which is the causative factor for many abnormalities such as retinal tear/detachment. It is also performed to remove abnormalities present in the vitreous gel which have led to vision loss (e.g. vitreous hemorrhage, retained lens fragment).
What to expect?
Vitrectomy surgery is almost always done in an outpatient setting (surgery center or hospital), meaning the patient goes home 1-3 hours after surgery. Since it is a surgical procedure, patients need to get medically cleared by their primary care doctor or an urgent care (if urgent). Surgery is generally performed under local anesthesia (i.e. patient is awake but the eye is anesthetized via local retrobulbar lidocaine/marcaine). This allows for the fastest and safest surgery with essentially no risk systematically. The retina specialist performs very small incisions in the sclera that do not require placement of stitches afterwards (i.e. small incision sutureless surgery). Depending on the type of condition, the surgery can last anywhere between 10-60 minutes. Once the surgery is completed, the patient’s eye will be patched until their post op visit which is usually within 48 hours following surgery. At the first postoperative visit, the patch is removed and instructions including use of eye drops is given. Following surgery, often special positioning (e.g. face down) is required in order for the retinal condition to be managed.
Vision following surgery will be hindered from a day to 6 weeks depending on the vitreous substitute utilized. There is typically very minor discomfort following surgery lasting 24-48 hours. It is extremely rare to have severe pain following surgery; if that happens or there is any vision loss, patients are to contact the doctor immediately.
What are the restrictions after vitrectomy surgery?
You may return to work in about 1 to 2 weeks. If your work involves physical activity or driving, you will need to restrict your activities and remain home longer. You may watch TV, read. Reading may be uncomfortable for several days, but using the eyes will not cause any damage.
What activities to avoid after vitrectomy?
If no positioning is required, avoid strenuous activity (weight lifting & swimming) for two weeks. Watching TV and reading will cause no harm. Your vision will remain blurred / poor for several weeks. Often the vision is distorted after surgery.
Can I bend over after a vitrectomy?
Avoid any bending or lifting for 1 week after surgery. After 1 week, you may do light housework and bend over to pick up light objects. Then, gradually resume your regular activities.
How long does it take for vision to return to normal after vitrectomy?
In most cases, it takes around 2 to 4 weeks for the vision to become clear after the vitrectomy. The extent of the clarity of the eyesight after the surgery depends on several factors, including: During vitrectomy, multiple incisions may be taken on the white of the eye called the sclera.
What happens if you don’t face down after vitrectomy?
Your surgery may not work if you do not recover in the recommended position. This is because lying in the wrong position puts pressure on other parts of your eye. That can lead to other eye problems. You cannot fly in an airplane, go to mountains/high altitudes or scuba dive until the gas bubble is gone.
What is the most common complication of vitrectomy?

What are the risks of vitrectomy?
- Infection.
- Excess bleeding.
- High pressure in the eye.
- New retinal detachment caused by the surgery.
- Lens damage.
- Increased rate of cataract formation.
- Problems with eye movement after surgery.
- Change in refractive error.
Is vitrectomy surgery risky?
A vitrectomy is a low-risk procedure with a high chance of success that can treat many eye conditions. In some cases, your vision may improve if substances or blood in your vitreous were causing you to have clouded or blurry vision
Why is my vision still blurry after vitrectomy?
Because of this, many patients are concerned when surgery is complete and they are still experiencing blurry vision. However, this is a normal side effect of a vitrectomy. It can take several days, or even several weeks, for the eyes to fully recover and for the vision to be restored to its full potential
How successful is pars plana vitrectomy?
Primary anatomical success rates of PPV range from 78% to 97% in the literature
How do you walk after a vitrectomy?
The best thing to do is to simply relax in bed or in a chair with both eyes closed. You can walk around the house if necessary, but be aware that your balance may be affected by having one eye closed, so move slowly to minimize the risk of a fall. After the first 48 hours, you can slowly increase your activity levels.
Does vision get worse after vitrectomy?
People who have had vitrectomy surgery will experience temporary poor vision while the eye is filled with gas, but if the surgery is successful the vision will improve as the gas reabsorbs and is replaced with the eye’s own clear fluid
What fills the eye after vitrectomy?
The eye is left filled with sterile saline (salt water) or with a vitreous substitute such as a gas bubble or silicone oil. When a vitreous substitute is used, a period of post-operative positioning (typically face-down) by the patient helps the retina heal.
What are the side effects of vitrectomy?
After a vitrectomy, there is a chance you might get:
- Cataracts.
- Raised pressure inside the eye.
- More bleeding in your vitreous.
- Retinal detachment.
- Infection.
- Problems moving your eyes.
Why is my vision still blurry 3 weeks after vitrectomy?
Answer: It is not uncommon to still have blurry vision for several months after retinal detachment surgery. This could be related to a small amount of residual fluid from the detachment that has not been completely reabsorbed yet.
When can I wash my hair after vitrectomy?
You can shower and wash your hair from the day after your procedure, however, it is advisable not to allow water to enter the eye for approximately 2 weeks following surgery.
How long does it take for a retina to reattach?
For those that have recently undergone laser surgery for a retinal tear or detachment, the healing process could take anywhere from one week to four weeks. It normally takes a full week for the laser treatment to fully seal the tear and prevent detachment, but things can still go wrong once sealed.
What not to do after a vitrectomy?
Don’t do things that might cause you to move your head. This includes moving quickly, lifting anything heavy, or doing activities such as cleaning or gardening. If your doctor used an oil or gas bubble to hold the retina in place, keep your head in a certain position for a few days or longer after the surgery.
How long after retina surgery can you fly?
Following retinal detachment surgery, it is important that flying is completely avoided until your eye has fully healed. This is usually for 3 to 4 weeks after surgery but possibly longer after some retinal detachment surgeries. Sometimes during surgery, a gas bubble is used to help keep the retina in place.
How long does the oil bubble stay in eye after vitrectomy?
In some cases, a gas or silicone oil bubble is placed in the eye. The gas bubble is gradually absorbed and is replaced by the eye’s own fluid. This gas may stay in the eye for up to eight weeks.
What is the patient’s part in treatment?
Treatment for glaucoma requires teamwork. Your ophthalmologist can prescribe treatment for glaucoma, but only you can make sure to follow your doctor’s instructions and use your eyedrops.
Once you are taking medication for glaucoma, your ophthalmologist will want to see you regularly. Typically, you will need to follow up every three to four months, depending on treatment needs.
What is a retinal tear?
A retinal tear or break happens when the gel-like vitreous in your eye pulls on your retina and causes a split. Your retina is a thin layer of tissue that’s sensitive to light found at the back of your eye.
A retinal tear isn’t the same as a retinal detachment. A retinal tear could lead to a retinal detachment if the tear isn’t treated. A retinal detachment happens when the retina pulls away from the tissues that support it.
You can also develop a hole in your retina when your retina gets thinner. Retinal holes are less likely to lead to retinal detachment.
Retinal tears and any injury that damages your retina threatens your eyesight and is a medical emergency. Contact your eye care provider as soon as you have retinal tear symptoms or any type of eye injury.
What are the symptoms of a retinal tear?
Symptoms of a retinal tear may include:
- Flashes of light (photopsia).
- Suddenly seeing more black spots or floaters than usual.
- Darkening vision.
- Blurred vision.
You might have a retinal tear and have no symptoms.
What causes a retinal tear?
Retinal tear causes include:
- Posterior vitreous detachment.
- Eye injuries.
- Eye surgeries.
What are the risk factors for retinal tears?
Risk factors for retinal tears include:
- Getting older.
- Being nearsighted (having myopia).
- Having a retina that’s thinning.
- A family history of retinal detachment or tears.
What are the complications of a retinal tear?
Retinal tears can become retinal detachments, which can cause vision loss if they’re not treated.
How do providers diagnose a retinal tear?
Your provider needs to be able to see clearly to the back of your eye during the eye exam. They’ll give you drops to widen your eyes (dilate them). Then they’ll use a special lens that’ll let them see your retina at the back of your eye.
How do eye care providers treat a retinal tear?
If you have a retinal tear, your eye care provider could recommend a retina specialist to do a laser procedure or cryopexy.
What is Laser surgery to treat retinal tears?
With this procedure, your retina specialist will use a laser to repair the retinal tear by surrounding it, preventing it from getting bigger. It also prevents fluid from getting behind the tear. This treatment has another name — photocoagulation. The laser burns your tissue and makes scars that cause the tear to heal.
The repair means that fluid won’t collect behind the break and won’t turn the torn piece into a full-scale retinal detachment.
Photocoagulation takes about 15 minutes.
What is Cryopexy to treat retinal tears?
With cryopexy, your provider will use a freeze treatment to seal the retinal tear. The goal is the same as with a laser procedure — to stop fluid from pushing the retina away from the tissue that supports it. With cryopexy, the extreme cold creates scar tissue and makes the seal.
Cryopexy takes about 30 minutes.
Complications/side effects of repairing retinal tears
Any type of surgical procedure has potential risks. With a laser procedure or cryopexy, you may have these complications:
- Bleeding in your eye.
- Cataracts.
- Needing surgery.
- Mild headache afterward.
How long does it take to recover from retinal tear repair?
You may have to wear an eye patch during a time specified by your provider. You should be able to drive and go back to work, unless your job means that you have to lift heavy things or participate in strenuous activities. It may take weeks for your eye to heal enough to do those things.
Can I prevent a retinal tear?
You really can’t prevent a retinal tear, but you can do things to protect your eyes and sight, including:
- Making and keeping eye care appointments: Eye exams protect your eye health. If you have nearsightedness, eye exams are especially important. Myopia makes you more prone to retinal detachment. Your eye care provider should include dilated exams to find small retinal tears.
- Protecting your eyes: Use safety goggles or other protection for your eyes when playing sports or doing other risky activities.
- Getting prompt treatment for any type of eye injury or changes: If you have an eye injury or notice blurred vision or other issues, see your eye care provider right away or go to the emergency room (ER).
- Managing your health: Take care of chronic conditions, choose nutritious foods in moderation and exercise regularly.
What can I expect if I have a retinal tear?
If you have treatment, or if your retinal tear heals on its own, your prognosis is good. If the tear is large and untreated, it could get worse and cause a retinal detachment. That condition is a medical emergency.
When should I see a Eye healthcare provider or ophthalmologist?
If you’ve had treatment for a retinal tear and you have any issues afterward, contact your eye doctor or go to an emergency room. These types of issues include:
- Severe pain.
- A loss of vision.
- Signs of infection, such as pus, swelling or fever.
What is a retinal hemorrhage?
A retinal hemorrhage is the medical term for bleeding in your retina. Hemorrhages are any type of bleeding from a damaged blood vessel. Retinal hemorrhages can be caused by traumas (like getting hit in the head) and health conditions that affect your eyes or blood vessels.
Most people have a retinal hemorrhage in only one eye at a time (a unilateral retinal hemorrhage). It’s less common, but it’s also possible to develop retinal hemorrhages in both eyes at the same time (bilateral retinal hemorrhage).
Some people never know they have a retinal hemorrhage and don’t experience any symptoms. Others lose vision. The damage can be permanent depending on what causes a retinal hemorrhage in your eye and how much bleeding there is.
Ophthalmologist, VR doctor (retina surgeon) treat a retinal hemorrhage depends on its cause. Many retinal hemorrhages don’t need treatment. You’ll need injections, laser treatment or surgery if you have a retinal hemorrhage that affects your vision or that could cause permanent blindness.
Visit your eye care specialist as soon as you notice any changes in your eyes or vision. Go to the emergency room (ER) if you suddenly lose the ability to see in one or both eyes.
What are the types of retinal hemorrhages?
Your eye care specialist will classify a retinal hemorrhage based on where it develops on your retina. Additionally, they might refer to the hemorrhage based on its shape or what it looks like. A retinal hemorrhage can also be multilayered — a retinal hemorrhage that affects more than one part of your retina.
The most common types of retinal hemorrhages include:
- Intraretinal hemorrhages: Intraretinal hemorrhages are tears or breaks in the tissue of your retina itself. They’re sometimes called dot-and-blot hemorrhages.
- Retinal nerve fiber layer hemorrhages: The retinal nerve fiber layer (RNFL) is the group of nerve cells that connect your retina to your optic nerve. Flame hemorrhages, disc or Drance hemorrhages and splinter hemorrhages all affect the RNFL.
- Preretinal hemorrhages: Preretinal hemorrhages are tears in the membrane that separates your vitreous cavity from your retina. They’re sometimes referred to as boat-shaped or D-shaped hemorrhages.
- Vitreous hemorrhages: Your eyeballs are filled with vitreous gel — a gel made of water and collagen. Vitreous hemorrhages happen when your retina bleeds into the vitreous cavity in your eye.
Who gets retinal hemorrhages?
Anyone can experience a retinal hemorrhage. People with certain health conditions are more likely to develop one, including:
- High cholesterol (hyperlipidemia).
- High blood pressure (hypertension).
- Atherosclerosis.
- Diabetes.
- Macular degeneration.
People who take blood thinners like (aspirin or warfarin) have a higher risk of retinal hemorrhages.
Babies are sometimes born with a retinal hemorrhage. Around half of babies born via assisted delivery (like vacuum extraction and forceps delivery) have a retinal hemorrhage at birth.
It’s more common for adults older than 40 to experience a retinal hemorrhage as they develop common age-related eye problems.
What are the symptoms of a retinal hemorrhage?
Many people don’t experience any symptoms when they have a retinal hemorrhage.
If you do have symptoms, you’ll probably notice changes in your vision. The most common retinal hemorrhage symptoms include:
- Sudden vision loss.
- Your vision getting noticeably worse or blurry.
- Blind spots.
- Patches or spots of darkness in your vision.
Seeing flashes or floaters.
What causes retinal hemorrhages?
Trauma or health conditions that damage your eyes or blood vessels over time cause retinal hemorrhages. The most common causes of retinal hemorrhages include:
- Trauma.
- Vascular disease (conditions that affect your blood vessels).
- Autoimmune disorders.
Leukemia and infections like bacterial endocarditis can also cause retinal hemorrhages. People older than 40 are more likely to develop age-related eye conditions like macular degeneration that can cause retinal hemorrhages.
Even if you have a condition that can lead to a retinal hemorrhage, it doesn’t mean you’ll definitely develop one. Similarly, it’s possible to experience a retinal hemorrhage without knowing you have one of these conditions.
See your healthcare provider for regular checkups to help catch warning signs of a condition or issue that might cause a retinal hemorrhage in the future.
Visit your eye care specialist as soon as you notice any changes in your eyes or vision.
Trauma
Trauma that causes retinal hemorrhages includes:
- Eye injuries: Any injury that damages your head or eyes can damage the blood vessels in your retinas.
- Shaken baby syndrome: Shaking an infant or toddler can cause bleeding in their brain and retinas.
- Altitude sickness: Moving to a higher elevation too fast can change the pressure in your eyes fast enough to cause a retinal hemorrhage. This can also happen if you’re a scuba diver who ascends from deep water too quickly.
- Carbon monoxide poisoning: Carbon monoxide (CO) poisoning happens when you breathe in fumes that contain CO. You can get very sick or even die if you breathe high levels of CO for even a few minutes.
Vascular disease
Conditions that damage or restrict your blood vessels can lead to a retinal hemorrhage. These conditions can be dangerous because they don’t usually cause symptoms until they’ve already damaged your blood vessels enough to cause complications. The most common types of vascular disease that cause retinal hemorrhages include:
- Hypertension (high blood pressure).
- High cholesterol.
- Retinal vein occlusions (RVOs).
- Postpartum preeclampsia.
- Anemia.
Autoimmune disorder
Autoimmune disorders happen when your immune system accidentally attacks your body instead of protecting it. It’s unclear why your immune system does this. Some types of autoimmune disorders can damage your retinas and cause retinal hemorrhages, including:
- Diabetes.
- Lupus.
- Vasculitis.
How are retinal hemorrhages diagnosed?
Your eye care specialist will diagnose a retinal hemorrhage with an eye exam. They’ll look at your eyes (including inside them) and perform a visual acuity test.
You might also need a few tests to diagnose what caused the retinal hemorrhage or to help your eye care specialist see how damaged your retina is. The most common tests you’ll need include:
- A blood test to check for signs of infections or to check your cholesterol.
- Angiography.
- Magnetic resonance imaging (MRI).
How are retinal hemorrhages treated?
How a retinal hemorrhage is treated depends on a few factors:
- What caused it.
- How much your vision is affected.
- How severe the bleeding in your retina is.
Many people don’t need treatment. If you have a small retinal hemorrhage that isn’t getting worse and isn’t affecting your ability to see, you’ll probably only need a few follow-up eye exams to make sure the hemorrhage is healing on its own. Your eye care specialist will tell you how often you’ll need your eyes checked.
If you do need treatment, you might need one of the following procedures:
- Laser or cryotherapy to repair the retinal hemorrhage.
- Surgery to normalize pressure in your eye or reattach your retina.
An injection of medication like anti-vascular endothelial growth factor (anti-VEGF) or a corticosteroid to reduce inflammation inside your eye.
How long does it take to recover from a retinal hemorrhage?
Your eye care specialist will tell you how long it’ll take to recover based on your specific symptoms and what caused the hemorrhage in your eye. Most people need a few weeks to recover from surgery to repair a retinal hemorrhage.
You’ll probably need to avoid medications like over-the-counter (OTC) NSAIDs (and any other anticoagulant medication that thins your blood) while you’re recovering. Talk to your ophthalmologist about what to expect.
How can I prevent a retinal hemorrhage?
The best way to prevent a retinal hemorrhage is to prevent conditions that cause them. Some steps you can take include:
- Eating a healthy diet low in saturated and trans fats, cholesterol, sodium (salt) and sugar.
- Exercising regularly.
- Maintaining a weight that’s healthy for you.
- Managing any health conditions, especially diabetes, high blood pressure and high cholesterol.
- Quitting smoking.
- Visiting a healthcare provider and eye care doctor regularly.
When should I have my eyes examined?
Having your eyes and vision checked regularly can help your eye care specialist identify problems right away. How often you should get your eyes checked usually depends on your age:
- Adults under 40: Every five to 10 years.
- Adults between 40 and 54: Every two to four years.
- Adults older than 55: Every one to three years.
You might need your eyes checked more often than this if you wear glasses, contacts or need another type of visual aid. People with diabetes need their eyes checked more often than what’s listed here.
Ask your eye care specialist how often you need an eye exam.
What can I expect if I have a retinal hemorrhage?
Many people make a full recovery from a retinal hemorrhage, even if they need surgery.
It’s possible for a retinal hemorrhage to cause permanent damage to your retina that affects your ability to see for the rest of your life. You might also have low vision after a retinal hemorrhage.
When should I see my eye and vision doctor?
See your healthcare provider or eye care specialist as soon as you notice any changes in your eyes or vision.
Go to the emergency room (ER) if you have any of the following symptoms:
- A sudden loss of vision.
- Severe eye pain.
- You see new flashes or floaters in your eyes.
What questions should I ask my doctor?
- What caused the retinal hemorrhage?
- Which type of retinal hemorrhage do I have?
- Will I need surgery?
- Will this affect my vision forever?
What is a retinal hemorrhage vs. a retinal detachment?
Retinal hemorrhages and retinal detachment are both serious issues that affect your retina.
A retinal hemorrhage is any injury or damage to your eye that makes blood vessels in your retina break or bleed. They can be caused by lots of other conditions and can happen suddenly (during trauma) or over time from a condition like vascular disease.
Retinal detachment (a detached retina) happens when your retina pulls away from the tissue at the back of your eye that supports it. It can cause a retinal hemorrhage. A detached retina usually isn’t painful. You’ll notice changes in your vision like bright flashes of light, darkened peripheral vision or a sudden loss of sight in one eye. Trauma and conditions that cause fluid buildup in your eye, like uveitis, can cause retinal detachment.
Go to the emergency room if you lose vision in one or both of your eyes or if you see new eye flashes and floaters.
What is a retinal hemorrhage vs. a subconjunctival hemorrhage?
Retinal hemorrhages and subconjunctival hemorrhages are both bleeding in your eye. The difference is where the hemorrhage is.
Retinal hemorrhages affect the retina — the layer of cells at the back of your eye.
A subconjunctival hemorrhage is a broken blood vessel on the surface of your eye. The conjunctiva is a thin, clear membrane that protects your eye.
What is retinal vein occlusion?
Retinal vein occlusion (RVO) is a partial or total blockage in a vein that drains blood from your retina. Your retina is a layer of tissue at the back of your eye that helps translate light into images you can see. A blockage in a retinal vein prevents blood from leaving your retina. This can lead to complications, including raised pressure in your eye and swelling. These issues need prompt treatment to prevent or minimize vision loss.
There’s no current safe way to unblock the vein. However, treatment can manage complications and protect your vision.
Eye care specialists tailor treatment to your individual needs. You may need multiple treatments ranging from injections to surgery to manage your condition.
Types of retinal vein occlusion
There are two types of RVO:
- Central retinal vein occlusion (CRVO), or blockage of the main retinal vein.
- Branch retinal vein occlusion (BRVO), or blockage of one of the smaller branch veins. This type is more common.
How common is retinal vein occlusion?
Retinal vein occlusion is the second most common disorder affecting your retina (diabetes-related retinopathy is the most common).
Researchers estimate that globally:
- Retinal vein occlusion affects over 16 million people.
- Central retinal vein occlusion affects between 1 and 4 in 1,000 people.
- Branch retinal vein occlusion affects between 6 and 12 in 1,000 people.
What are the symptoms of retinal vein occlusion?
Symptoms of retinal vein occlusion typically affect one eye and include:
- Blurry vision or vision loss: This may start suddenly or develop gradually over a period of hours or days.
- Floaters: These are dark spots or lines in your field of vision.
- Pain or pressure in your eye: This is typically in more severe cases.
You may not have any symptoms until complications arise. Some people don’t realize there’s a problem until their provider finds the issue during a routine eye exam.
What causes retinal vein occlusion?
A disruption to normal blood flow through your retinal vein causes this condition. The disruption may happen due to:
- A blood clot.
- A slowdown of blood flow.
- Compression of your retinal vein at the point where it crosses paths with your retinal artery. Your retinal artery supplies oxygen-rich blood to your retina. Your retinal artery may grow stiff from aging or plaque buildup, and it may press on your retinal vein. This can damage the inner lining of your retinal vein, creating conditions where a blood clot is more likely to form.
What are the risk factors for retinal vein occlusion?
Being over age 40 is a major risk factor. RVO usually affects people in their 50s or 60s. However, this condition can also affect people younger than age 40.
Having certain medical conditions can also raise your risk. These include:
- Atherosclerosis.
- Diabetes.
- Glaucoma.
- High blood pressure.
Prior history of retinal vein occlusion in one eye raises your risk of developing the condition in your other eye.
What are the complications of retinal vein occlusion?
Retinal vein occlusion can lead to complications such as:
- Cystoid macular edema: This is swelling in the center of your retina (macula). It can cause blurry vision or loss of vision.
- Neovascularization of the eye: Abnormal blood vessels can form in different parts of your eye, typically your iris (rubeosis iridis). This happens in about 1 in 4 people with RVO. Abnormal blood vessels less commonly form in your retina.
- Bleeding in your eye (vitreous hemorrhage): This is when blood leaks into your vitreous humor, the gel-like substance that fills your eyeball. It results from the formation of abnormal blood vessels, which are prone to leaking.
- Neovascular glaucoma: Abnormal blood vessels in your eye can cause pain and a dangerous increase in pressure inside your eye.
- Retinal detachment: Abnormal blood vessels in your retina may cause your retina to pull away from the tissues that support it.
People with RVO have a higher risk of cardiovascular diseases, including stroke, compared to people without RVO. This may be due to shared underlying risk factors like high blood pressure and atherosclerosis.
How is retinal vein occlusion diagnosed?
Eye care specialists diagnose RVO through an eye exam and retinal imaging tests. They also coordinate care with your primary care physician (PCP) to discover the cause of blood flow problems.
Eye exam
Your eye care specialist will dilate your pupils so they can see into the back of each eye. They’ll use a microscope and a head-mounted ophthalmoscope to shine a light into your eye. They’ll closely examine the inside of your eye to look for complications and signs of vision loss.
This exam can help:
- Distinguish between central and branch RVO.
- Identify signs of macular edema and abnormal blood vessel formation.
- Estimate how much of your retina lacks blood flow.
You may need further testing to diagnose RVO and show the extent of complications.
Tests to diagnose retinal vein occlusion
Your eye care specialist may use one or more of the following tests to help diagnose and describe your condition:
- Fundus photography: This form of retinal imaging shows the presence of abnormal new blood vessels and the amount of bleeding inside your eye.
- Optical coherence tomography (OCT): This form of high-resolution imaging shows the presence of macular edema. It measures the thickness of your retina and provides precise numbers that help guide the treatment of your condition over time.
- Fluorescein angiography: For this test, your provider injects dye into a vein in your arm. The dye travels to the blood vessels in your retina and makes them stand out in imaging. Your provider may use this form of imaging to show the extent of a blockage in your retinal vein. This test also shows how much of your retina isn’t receiving adequate blood flow.
Coordinated care Your eye care specialist and primary care physician will work together to find the cause of RVO and lower your risk for future issues. You may need blood tests to check your cholesterol levels, blood sugar and other important numbers.
What are the treatments for retinal vein occlusion?
There’s currently no way to reverse or cure the blockage in your retinal vein. But eye care specialists can prevent or treat the complications of retinal vein occlusion with:
- Anti-VEGF injections.
- Steroid injections.
- Panretinal photocoagulation (PRP).
- Vitrectomy surgery.
- Medications to manage risk factors.
The goals of treatment are to:
- Improve your vision or prevent it from getting worse.
- Identify and treat complications that can harm your vision and eye health.
- Manage risk factors to prevent future problems.
Your provider will combine treatment options as necessary and explain the timing for each.
Anti-VEGF injections
This is a first-line (first-choice) treatment for people with macular edema. VEGF stands for vascular endothelial growth factor. This is a protein that spurs new blood vessel growth (angiogenesis). Too much VEGF can lead to the formation of abnormal blood vessels that can leak and cause swelling.
Anti-VEGF injections interrupt the production of VEGF in your eye to reduce swelling. Your provider gives you eye drops to numb your eye and reduce pain before injecting the medication into the gel-like substance (vitreous humor) that fills your eyeball. You may need injections at regular intervals for one to two years depending on your condition.
Steroid injections
Injections of steroid medication into your eye can also help reduce swelling. However, in some people, steroid injections cause elevated eye pressure and cataracts. So, they’re often a second-line treatment when anti-VEGF injections aren’t adequate.
Panretinal photocoagulation (PRP)
This laser surgery creates small burns in areas of your retina that lack blood flow. Doing so decreases the number of proteins (VEGF) that promote the formation of abnormal blood vessels. Reducing VEGF helps prevent neovascularization and related bleeding in your eye. It also helps keep your intraocular pressure stable.
Vitrectomy surgery
Posterior pars plana vitrectomy (PPV) is a surgery that helps people with retinal vein occlusion who have:
- Severe bleeding in their eye (vitreous hemorrhage).
- Bleeding that lasts more than four weeks.
- Bleeding that keeps coming back.
- Retinal detachment.
Surgery removes vitreous humor from your eye and repairs damage to your retina.
Medications to manage risk factors
Many people with retinal vein occlusion have underlying conditions like high blood pressure, diabetes or high cholesterol. These conditions can raise your risk of blood vessel problems. Your eye care specialist will work together with your primary care physician (PCP) to tailor treatment to your needs. Your PCP may prescribe medications to:
- Lower your blood pressure.
- Manage your cholesterol levels.
- Address other issues.
Can I prevent retinal vein occlusion?
Learning you’re at risk for retinal vein occlusion is the first step toward preventing it. Talk to your ophthalmologist about your level of risk and how to lower it.
It’s also important to talk to your primary care physician about underlying conditions that raise your risk for blood flow problems. They’ll recommend treatments as needed to manage those conditions and help keep your eyes — and whole body — healthy.
Specific things you can do to lower your risk include:
- Follow a diet that supports your heart and blood vessel health.
- Make exercise part of your daily routine.
- Keep a weight that’s healthy for you.
- Avoid smoking and all tobacco products.
What can I expect if I have this condition?
Your prognosis depends on many factors, including the location of the blockage and complications that arise. Some people have permanent vision damage, while others have vision that gradually gets better over time. Your eye care specialist is the best person to tell you exactly what you can expect in your individual situation.
Your provider may refer you to vision rehabilitation. This is a form of rehab that teaches you techniques for living with reduced vision. These may include using devices like magnifying glasses or assistive-computer technology. Your provider may also refer you to a social worker who can help you cope with lifestyle changes.
How do I take care of myself?
Living with retinal vein occlusion (RVO) can be stressful because you may need:
- Multiple eye injections
- Multiple laser treatments.
- Many follow-up appointments.
- Help getting to and from your appointments (if your condition or treatment prevents you from driving safely).
All of this may take a toll and feel overwhelming to you. Remember that your healthcare team is there to help you.
Talk to your providers about how you’re feeling. They may suggest resources to help you learn more about your condition and why all of this effort is so important. They may also connect you with support groups or other community resources where you can talk to people who are in a similar situation. Learning from others’ experiences and sharing your own can help make everything feel more manageable.
When should I seek medical care?
Your eye care specialist will tell you how often you need appointments for monitoring or treatment. Call them if you experience new or changing symptoms or have questions about your treatment plan.
When should I go to the emergency room?
Call 911 or your local emergency number if you have symptoms of a retinal detachment. This is a medical emergency that requires prompt care.
What questions should I ask my Ophthamologist?
You may want to ask your eye care specialist:
- What caused the blockage in my retinal vein?
- What treatments are best for me?
- What are the benefits and risks of each treatment?
- What follow-ups will I need?
- How will this condition affect my vision?
- What is my outlook?
What is retinal detachment?
Retinal detachment is a painless but serious eye condition. It happens when your retina, the layer of tissue at the back of your eye, detaches from the tissues that support it. A detached retina affects your vision and can lead to blindness.
Your retina senses light and sends signals to your brain so you can see. When your retina pulls away from the tissues that support it, it loses its blood supply. The blood vessels in those tissues carry nutrients and oxygen to your retina.
Call your eye care provider or go to the emergency room (ER) right away if you notice:
- More eye floaters than usual.
- Flashes of light
- A shadow in your vision.
These can be symptoms of a detached retina. Don’t wait to see if you feel pain. Your provider will want to start treatment as soon as possible.
Types of retinal detachment
There are three types of retinal detachment:
- Rhegmatogenous: This is the most common type and usually happens as you get older. A small tear in your retina lets the gel-like fluid called vitreous humor travel through the tear and collect behind your retina. The fluid pushes the retina away, detaching it from the back of your eye. As the vitreous shrinks and thins with age, it pulls on the retina, tearing it.
- Tractional: In this type of detached retina, scar tissue on your retina can pull it away from the back of your eye. Diabetes is a common cause of these retinal detachments. Extended periods of high blood sugar can damage blood vessels in your eye and cause scar tissue. The scars and areas of traction (pulling) can get bigger, tugging your retina away from the back of your eye.
- Exudative: This type of retinal detachment happens when fluid builds up behind the retina even though there’s no retinal tear. As the fluid collects, it pushes your retina away from supporting tissue. The main causes of fluid buildup are leaking blood vessels or swelling behind the eye, which can happen from conditions like uveitis (eye inflammation).
How common is retinal detachment?
Estimates for the incidence of retinal detachment vary. (The incidence is the number of new cases in a set period of time, usually a year.) One figure estimates incidence in the U.S. at 1 in 10,000 people. Another study estimates the annual risk of Rhegmatogenous retinal detachment, the most common type, at 6.3 to 17.9 per 100,000 people.
What are the symptoms of retinal detachment?
Some people don’t notice any symptoms of retinal detachment, while others do. It depends on severity — if a larger part of the retina detaches, you’re more likely to experience symptoms.
Symptoms of a detached retina can happen suddenly and include:
- Seeing flashes of light (photopsia).
- Seeing a lot of floaters — flecks, threads, dark spots and squiggly lines that drift across your vision. (Seeing a few here and there is normal and not cause for alarm.)
- Darkening of your peripheral vision (side vision).
- Darkening or shadow covering part of your vision.
What are the causes of and risk factors for retinal detachment?
Risk factors and causes for detached retinas include:
- Aging.
- Eye injury.
- Having a previous retinal detachment or a family history of retinal detachment.
- Having a previous eye surgery.
Having certain eye conditions also raises your risk for retinal detachment, such as:
- Being very nearsighted.
- Posterior vitreous detachment, where the thick fluid in the middle of the eye (vitreous) pulls away from the retina.
- Other conditions that affect your retina or choroid, like lattice degeneration (retina thinning) or diabetes-related retinopathy.
- Certain inherited eye disorders
- A history of retinal tears or detachments in the other eye.
If you’re at high risk for retinal detachment, talk to your healthcare provider. Your provider can help you set an eye exam schedule and suggest other steps to protect your eye health.
What are the complications of this condition?
Having a detached retina is a serious condition that can cause loss of vision. Permanent blindness can happen as quickly as a few days.
How do providers diagnose retinal detachment?
You need an eye exam to diagnose retinal detachment. Your eye care provider will use a dilated eye exam to check your retina. They’ll put eye drops in your eyes. The drops dilate, or widen, the pupil. After a few minutes, your provider can get a close look at the retina.
Your provider may recommend other tests after the dilated eye exam. These tests are noninvasive. They won’t hurt. They help your provider see your retina clearly and in more detail:
- Optical coherence tomography (OCT): Most often, you’ll get dilating eye drops for this imaging. Then you sit in front of the OCT machine. You rest your head on a support so it stays still. The machine scans your eye but doesn’t touch it.
- Fundus imaging: Your provider may take wide-angle images of your retina. Your provider usually dilates your eyes for this test.
- Eye (ocular) ultrasound: You won’t need dilating drops for this scan, but your provider may use drops to numb your eyes so you won’t feel any discomfort. You sit in a chair and rest your head on a support, so it stays still. Your provider gently places an instrument against the front of your eye to scan it. Next, you sit with your eyes closed. Your provider puts gel on your eyelids. With your eyes closed, you move your eyeballs as your doctor scans them with the same instrument.
- Computed tomography (CT scan): This imaging test combines X-rays with a computer and is usually used if there’s a history of trauma or possible penetrating eye injury.
How do you treat retinal detachment?
Your eye care provider will discuss treatment options with you. You may need a combination of treatments for the best results.
Treatments include:
- Laser therapy or cryopexy.
- Pneumatic (gas bubble) retinopexy.
- Scleral buckle.
- Vitrectomy.
Laser (thermal) therapy or cryopexy (freezing)
Sometimes, your provider will diagnose a retinal tear before the retina starts pulling away. Your provider uses a medical laser or a freezing tool to seal the tear. These devices create a scar that holds the retina in place.
Pneumatic retinopexy
Your provider may recommend this approach for the right candidates. During pneumatic retinopexy:
- Your provider injects a small gas bubble into the eye.
- The bubble presses against the retina, closing the tear.
- You may need laser or cryopexy (freezing) to seal the tear.
- Your body reabsorbs the fluid that collected under your retina. Your retina can now stick to your eye wall the way that it should. Eventually, your body also absorbs the gas bubble.
After surgery, your provider will recommend that you keep your head still for a few days to promote healing. Your provider may also tell you what position you should lie in or sleep in.
These recommendations may seem uncomfortable or annoying, but they’re particularly important. It’s a short-term sacrifice for long-term benefits.
Scleral buckle
During a scleral buckle surgery:
- Your provider surgically places a silicone band or sponge (buckle) around the eye.
- The band holds the retina in place and stays there permanently. You can’t see the band.
- Your provider seals the tear with a laser or cryopexy.
- Your provider may inject a gas bubble or drain the fluid under the retina to help reattach it.
Vitrectomy
During a vitrectomy, your provider:
- Surgically removes the vitreous.
- Uses laser or freezing to seal all retinal tears or holes.
- Places a bubble of air, gas or oil in the eye to push the retina back in place.
If your provider uses an oil bubble, you’ll have it removed a few months later. Your body reabsorbs gas and air bubbles. If you have a gas bubble, you may have to avoid activities at certain altitudes. The altitude change can increase the size of the gas bubble and the pressure in your eye. You’ll have to avoid flying and traveling to high altitudes. Your provider will tell you when you can start these activities again.
Complications/side effects of treating retinal detachment
While surgery to reattach your retina is often very successful, any surgery can have risks or complications. These risks and complications include:
- Bleeding.
- Infection.
- Higher pressure in your eye (intraocular pressure).
- The chance that you may need another surgery.
- Membranes that form after surgery that can shrink and pull tissues out of place. The name for this is proliferative retinopathy or epiretinal membrane.
- Rapid cataract formation that requires additional cataract surgery.
What can I expect after retinal detachment surgery?
After treatment for a detached retina, you may have some discomfort. It can last for a few weeks. Your retina specialist will discuss pain medicine and other forms of relief. You’ll also need to take it easy for a few weeks. Talk with your specialized retina doctor about when you can exercise, drive and get back to your regular activities.
Other things you can expect after surgery:
- Eye patch: Wear the eye patch for as long as your provider tells you to do so.
- Head position: If your retina surgeon put a bubble in your eye, follow instructions for your head position. Your provider will let you know the position your head should be in and how long to keep it there to help heal your eye.
- Eye drops: Your retina consultant will instruct you on how to use the drops to help your eye heal.
- Improved vision: About four to six weeks after surgery, you’ll start to notice your eyesight improving. It may take a few months until you notice the full effects.
Can I prevent retinal detachment?
You can’t prevent Rhegmatogenous retinal detachment, but you can take steps to lower your risk:
- Get regular eye care: Eye exams protect your eye health. If you have nearsightedness, eye exams are especially important. Myopia makes you more prone to retinal detachment. Your eye care provider should include dilated exams to find small retinal tears.
- Stay safe: Use safety goggles or other protection for your eyes when playing sports or doing other risky activities.
- Get prompt treatment: If you notice detached retina symptoms, see your eye care provider right away or go to the emergency room.
- Maintain your overall health: Manage chronic conditions, eat balanced meals and get regular exercise.
You can help to prevent diabetes-related tractional retinal detachment by improving your blood glucose levels and blood pressure.
How often should I get regular eye exams?
People who have an average risk of eye disease should get eye exams once a year. If you’re at higher risk for eye disease, you may need checkups more frequently. Talk to your provider to figure out your best exam schedule.
What can I expect if I have a retinal detachment?
Your outlook depends on factors like how clear your vision was before the retinal detachment, how extensive your detachment was and if there are any other complicating factors. Your retina specialist will talk to you about what type of vision improvement you can expect.
In general, surgery for rhegmatogenous retinal detachment is highly successful — the repair works about nine out of 10 times. Sometimes, people need more than one procedure to return the retina to its place.
Can I get a detached retina again?
It’s possible to get a detached retina more than once. You may need a second surgery if this happens. Talk to your retina doctor about preventive steps you can take to protect your vision.
How do I take care of myself?
It’s essential that you follow the instructions you get from your eye care provider about positioning and about your activities.
Ask your provider for suggestions on how to make things easier, like using a firm neck pillow to help keep your head in place. If you must lie face down or stay in that position for most of your time, your provider’s office can help you get face-down equipment for your home.
When should I go to the emergency room?
Your surgeon’s instructions will list situations that are emergencies, but you should contact your provider or get emergency help if you:
- Have severe, unexpected pain.
- Have symptoms of an infection, such as swelling or a fever.
- Have unexpected discharge from your eye.
Have a sudden decrease in your ability to see.
What questions should I ask my eye care provider?
If you have retinal detachment (or face a higher risk), ask your provider:
- Which retinal detachment treatment is best for me?
- Will I need surgery?
- How can I protect my eye health after surgery?
- How often should I have eye exams?
- What else can I do to lower my risk of retinal detachment?
What is diabetic retinopathy?
The retina is a layer of tissue inside the back of your eye. If you have diabetes, the tiny blood vessels in your retina can slowly become damaged. This causes problems with your sight.
What are the symptoms of diabetic retinopathy?
You might not notice any symptoms in the early stages. Therefore, it is important to get your eyes checked regularly by an optometrist if you have diabetes.
If you have diabetic retinopathy, you might:
- find that your vision fluctuates (gets better and worse)
- have blurred or distorted vision
- have patchy vision that can’t be corrected with prescription glasses
- become sensitive to light or glare
- have eye floaters (moving specks) in your vision
- find it more difficult to read, watch television or drive
What causes diabetic retinopathy?
Diabetic retinopathy is a complication of diabetes. Diabetes can cause the tiny blood vessels in the back of your eye to swell and bleed.
This process can slowly damage your retina. Usually, both eyes are affected.
The longer you have diabetes, the more likely it is that you will get diabetic retinopathy.
Your chance of getting diabetic retinopathy also increases if:
- your diabetes and blood sugar levels are not well controlled
- you have high blood pressure
- you have high cholesterol
How is diabetic retinopathy diagnosed?
Diabetic retinopathy is diagnosed by an eye test.
At the eye test the optometrist will examine your eyes. They may use eye drops to help to see the back of your eye. They may take a photo of the back of your eye.
If you have diabetes, you should have your eyes checked when your diabetes is first diagnosed and then at least once every 2 years.
If you experience any changes to your vision, see an optometrist or ophthalmologist as soon as you can.
How is diabetic retinopathy treated?
Treatment for diabetic retinopathy can slow or prevent vision loss. It is best to start treatment as soon as you can.
Keeping your blood sugar and blood pressure under control can help. Eating a healthy diet and getting regular exercise are useful as part of managing your diabetes.
Other treatments include:
- laser treatment to seal leaking blood vessels and stop the growth of abnormal blood vessels
- surgery, such as vitrectomy
- medicines that can reduce swelling in the retina
Can diabetic retinopathy be prevented?
You can reduce your chance of getting of diabetic retinopathy by :
- keeping your blood glucose levels, blood pressure and cholesterol levels in a healthy range
- not smoking
- having regular eye checks with your optometrist so that any early changes can be found and treated
What is strabismus (adult)?
Strabismus (or ‘squint’) is where one of your eyes points in towards your nose (convergent) or out towards your ear (divergent). Sometimes one eye may point up or down. Strabismus may be present all the time or only sometimes.
How does strabismus happen?
Strabismus in adults can happen because of disease that affects your eye muscles (such as thyroid eye disease and myasthenia), disease that affects the nerves to your eye muscles (such as high blood pressure and diabetes) or trauma (where a physical force is applied directly to your eye).
Strabismus can also be caused by trying to correct short- or long-sightedness, or by poor vision in one eye as a result of amblyopia (or ‘lazy eye’).
Strabismus may not cause any symptoms. For some people it can be serious.
What are the benefits of surgery?
The aim of surgery is to improve the alignment of your eyes and reduce or stop any double vision.
Are there any alternatives to surgery?
Glasses or contact lenses can sometimes be used to control strabismus by helping your eyes to focus.
Double vision can often be controlled by wearing glasses with special prism lenses.
What does the operation involve?

The muscles of the eye.
The operation is usually performed under a general anaesthetic but various anesthetic techniques are possible. The operation usually takes about 40 minutes.
Your surgeon will make a small cut on the surface membrane of your eye (conjunctiva). They will separate one or more eye muscles from the surface of your eyeball.
Using small dissolvable stitches, your surgeon will reattach the muscles, making them tighter or looser than they were before, depending on the correction that needs to be made.
How can I prepare myself for the operation?
Helping your surgeon
If you have adjustable stitches, you can help your surgeon by relaxing, listening carefully and following the instructions they give you.
Lifestyle changes
If you smoke, stopping smoking now may reduce your risk of developing complications and will improve your long-term health.
Try to maintain a healthy weight. You have a higher risk of developing complications if you are overweight.
Regular exercise should help to prepare you for the operation, help you to recover and improve your long-term health. Before you start exercising, ask the healthcare team or your GP for advice.
What complications can happen?
General complications of any operation
- bleeding
- infection
- allergic reaction to the equipment, materials or medication
- chest infection
Specific complications of this operation
- continued strabismus
- worse strabismus
- double vision
- a slipped or lost eye muscle, muscle scarring or making a hole in the eye with a needle
- reduced blood supply to the front of the eye
Consequences of this procedure
- scarring of the conjunctiva
- pain
How soon will I recover?
You should be able to go home after a few hours.
Do not swim or lift anything heavy until you have checked with your surgeon. Regular exercise should help you to return to normal activities as soon as possible. Before you start exercising, ask the healthcare team or your GP for advice.
Most people make a good recovery.
What is strabismus for child?
Strabismus (or ‘squint’) is where one of the eyes points in towards the nose (convergent) or out towards the ear (divergent). Sometimes one eye may point up or down.
How does strabismus happen?
Strabismus in children is usually related to how their eyes focus. The condition often runs in the family and affects 1 in 50 children under 5 years old.
Strabismus can also happen if the nerves to the eye muscles, or the eye muscles themselves, are not working properly.

The muscles of the eye.
What are the benefits of surgery?
Your child’s eyes should appear to move together. If your child had a divergent squint, their binocular vision may improve.
Are there any alternatives to surgery?
Glasses or contact lenses can help the eyes to focus.
If one eye is ‘lazy’, placing a patch on the good eye can train the affected eye to work so that vision develops normally in both eyes.
What does the operation involve?
The operation is performed under a general anaesthetic and usually takes about an hour.
Depending on the type of squint your child has, your surgeon will need to tighten or loosen one or more of the eye muscles.
Your surgeon will make a small cut on the surface membrane of the eye (conjunctiva). They will separate one or more eye muscles from the surface of the eyeball. Using small dissolvable stitches, your surgeon will reattach the muscles, making them tighter or looser than they were before, depending on the correction that needs to be made.
How can I prepare my child for the operation?
Your child should try to maintain a healthy weight. They will have a higher risk of developing complications if they are overweight.
What complications can happen?
General complications of any operation
- bleeding
- infection
- allergic reaction to the equipment, materials or medication
Specific complications of this operation
- continued strabismus
- worse strabismus
- double vision, in children over the age of 5
- a slipped or lost eye muscle, muscle scarring or making a hole in the eye with a needle
Consequences of this procedure
- pain
How soon will my child recover?
They should be able to go home after a few hours.
Your surgeon will tell you when your child can return to normal activities. Your child should not swim or do strenuous exercise until you have checked with your surgeon.
Most children make a good recovery.
What is the lacrimal apparatus?
The lacrimal apparatus is the medical name for your tear system. It’s a group of glands, sacs and ducts that makes new tears and drains old ones away. Each of your eyes has its own lacrimal apparatus.
Your tear system is a complex network that lubricates and protects your eyes. Visit an eye care specialist if you notice any changes in your eyes. If your eyes are too dry or too watery, there might be something interfering with your tear system.
What does the tear system do?
Your tear system is like an automatic irrigation system. Instead of sprinklers, underground plumbing and drains working together to keep your lawn green, your tear system has glands and ducts that move lacrimal fluid (the medical term for your tears) across your eyes.
Your eyes produce tears to protect themselves. They lubricate tissue like your conjunctiva and cornea. They also flush foreign materials (like allergens or dust) out of your eye. Your facial nerve — sometimes referred to as seventh cranial nerve — controls the muscles in your face and eye that pump tears into and out of your eye.
Tears are created in lacrimal glands in the upper outside corners of your eyes. They’re mostly salt and water. This fluid moves across your eyes as you blink and is mixed with oil from your meibomian glands to form your tears. This keeps the water from evaporating too quickly. Some of the oils stay along the edge of the eyelid to keep tears from “leaking” over your eyelashes.
Tears that have been flushed from your eyes drain away and into your tear ducts that empty into the back of your nose. That’s why you might feel stuffy if you’ve been crying. Your excess tears are flowing faster than they usually would into the back of your nose and draining into your throat.
What are the components of the tear system?
The components of your tear system include:
- Lacrimal glands (tear glands): Lacrimal glands behind the upper outside corner of your eyes make the salty water that becomes your tears. The glands are each about the size of an almond.
- Meibomian glands: Meibomian glands on the edges of your eyelids produce oil that mixes with the water from your lacrimal glands to become your tears. The oil helps the water cling together and stay in your eyes as long as it needs to.
- Lacrimal puncta: Lacrimal puncta are the openings that pump tears out of your eyes. You have a punctum (the singular form of puncta) in each of your upper and lower eyelids on the inside of your eye, near your nose. Every time you blink, your puncta act like valves that drain used tears away from your eye.
- Lacrimal sacs: Lacrimal sacs in the inside corner of your eye collect tears that drain out of your eyes through your lacrimal puncta. They act like temporary reservoirs for tears that have just left your eyes. They keep old tears from flooding your tear ducts constantly.
- Nasolacrimal duct (tear ducts): Nasolacrimal duct is the medical term for your tear ducts. Old tears that leave your eye through your lacrimal puncta and lacrimal sacs drain into tear ducts on either side of your nose. Your tear ducts empty into the back of your nose.
What are the most common conditions that affect my tear system?
Some of the most common conditions that affect your tear system include:
- Dry eyes.
- Watery eyes (epiphora).
- Blocked tear ducts (nasolacrimal duct obstruction).
- Dacryoadenitis.
- Dacryocystitis.
What are the most common signs or symptoms that something is wrong with my tear system?
Visit an eye care specialist if you have dry eyes or watery eyes. These are the most common signs that something’s interfering with your tear system.
If something is wrong with one part of your lacrimal apparatus, it can affect your whole tear system. For example, if something is blocking your meibomian glands, your tears might spill out of your eyes. This can make it feel like you’re making more tears than usual because they’re missing the oil that helps them stay in your eye.
Talk to an eye care specialist if you notice any changes in your eyes. Even a small change like frequent dry eyes can be a sign of an issue that an eye care specialist can diagnose and treat.
How do I take care of my tear system?
Visit an eye care specialist for regular eye exams. They’ll check your vision and the overall health of your eyes, including your tear system.
Tell your eye care specialist about any changes in your vision. If you wear glasses or contact lenses, have your eyes examined regularly so your provider can adjust your prescription as often as necessary. If you have diabetes, you need to see your eye care specialist at least once a year.
Make sure you’re wearing proper eye protection for any sport or activity that could cause an eye injury.
What is dry eye?
Dry eye is a condition that affects your tear film, the three layers of tears that cover and protect the surface of your eyes. You need a smooth and stable tear film to help you see clearly and comfortably. Disruptions to your tear film can cause uncomfortable symptoms like burning, itching, watering or blurred vision. Many different factors can prevent your tear film from working as it should and lead to dry eye. That’s why healthcare providers consider dry eye a multifactorial disease. Its causes and risk factors are numerous and complex. So, it may take a while to get to the root of the problem and figure out what’s causing your symptoms. If you have dry eye, it’s important to establish care with an ophthalmologist to manage your condition.
What is the Types of dry eye disease?
From its name alone, you might think dry eye disease simply means your eyes don’t produce enough tears. That’s actually only part of the story. There are several types of dry eye disease.
- Aqueous deficient dry eye: This is when your eyes don’t produce enough tears. Your lacrimal gland (in the upper, outer corner of each eye) produces your aqueous tears. These tears make up the middle, watery layer of your tear film. Some autoimmune conditions can cause inflammation in your lacrimal gland and prevent it from producing enough aqueous tears.
- Evaporative dry eye: This is when your tears evaporate too quickly. The most common cause is meibomian gland dysfunction. This means the glands in your eyelids that produce the outer, oily layer of your tear film don’t work properly. As a result, the oily layer is unstable and can’t protect the watery layer from drying up.
- Mixed dry eye: Some people have aqueous tear deficiency and tear instability. This means your eyes don’t produce enough tears, plus your tear film is unstable. Both of these problems lead to dry eye symptoms.
How common is dry eye disease?
Dry eye disease is common. Research estimates that 16 million people in the U.S. have dry eye. Around the world, dry eye affects tens of millions of people. It’s more common in Asia compared with North America and Europe. It’s also more common among people who’ve gone through menopause.
What can dry eye be a sign of?
Dry eye may occur on its own or along with other medical conditions. In some cases, dry eye is a sign of.
What are the symptoms of dry eye?
When you have dry eye, you might feel like there’s something in your eye that just won’t come out. This can feel like a scratchy, gritty or sandy sensation. Symptoms may also include:
- Burning or stinging.
- Feeling sensitive to light.
- Blurred or changed vision.
- Mucus that comes out of your eye.
- Watery eyes, with excess tears running down your cheeks.
The watery eyes symptom may seem confusing. But it’s a common aspect of dry eye. It happens when your meibomian glands aren’t making enough oils for the outer layer of your tear film. So, the middle, watery layer of your tear film evaporates too quickly. In response, your lacrimal glands try to make more watery tears to compensate. But these tears can’t properly coat your eye, as the oily layer would. So, they can’t solve the underlying problem.
What causes dry eye?
Dry eye happens when:
- Your eyes don’t produce enough tears.
- Your tears evaporate too quickly.
- Both of these happen together.
Many different factors can make you more likely to develop dry eye disease or have symptoms that get worse over time.
Risk factors for dry eye disease
Some risks you can’t control. For example, the older you get, the more likely you are to develop dry eye. But other risks you may be able to manage through lifestyle changes or adjustments to your medications.
Talk to your provider if you have any of the risk factors listed below. You may be able to make some changes to lower your risk for dry eye or lessen bothersome symptoms.
- Environment and lifestyle factors: Things like the weather, how much time you spend looking at screens, contact lens use, smoking or allergies can increase your risk of dry eye.
- Medications: Taking certain medications can increase your risk of dry eye, including some that treat depression, allergies, blood pressure, glaucoma, menopause and pain. Anticholinergics, oral contraceptives and systemic retinoids can increase your risk as well.
- Medical conditions: Many different neurological conditions, eye conditions, autoimmune conditions and endocrine conditions can raise your risk of dry eye.
- Surgeries: Some eye surgeries increase your risk of dry eye, including LASIK, cataract surgery and surgery on your cornea.
How is dry eye diagnosed?
Healthcare providers diagnose dry eye through your medical history, an eye exam and testing.
Medical history
Your provider may ask you to fill out a questionnaire to learn about your symptoms and medical history. You should be prepared to provide lots of information, including:
- Eye-related symptoms and how long you’ve had them.
- Environmental factors that make your symptoms worse.
- Other symptoms, including dry mouth, cavities, mouth ulcers, fatigue and joint pain.
- Allergies.
- History of eye diseases.
- History of other medical conditions, including allergies and chronic viral infections.
- History of surgeries.
- Whether you smoke or are around second-hand smoke.
- How often you wash your eyelids, and what products you use.
- History of trauma to your eye area.
Eye exam
Your provider will give you a thorough eye exam to check the health of your eyes and determine what’s causing your symptoms. During your exam, your provider:
- Looks for signs of dry eye.
- Looks for other possible causes of your symptoms, besides dry eye disease.
- Checks the health of your tear film (the three layers of tears that cover your cornea).
- Performs testing.
Tests that diagnose dry eye
There’s no single test that diagnoses dry eye. Rather, providers may use many tests, including:
- Slit lamp exam: This test checks the amount of tears your eyes produce. The provider shines a light into each of your eyes and uses a microscope to examine your eyes and eyelids.
- Schirmer’s test: This is another way to check your tear production. The provider places a tiny piece of paper along the edge of your eyelid and leaves it there for several minutes. Your eye produces tears in response, and your provider then measures those tears by looking at how much of the paper they cover.
- Tear breakup time (TBUT) test: This test checks how quickly your tears evaporate. The provider puts dye into your eye and uses a microscope to see how long your tear film remains stable (doesn’t break up). They measure the amount of time between your last blink and when the first dry area shows up on your cornea. A time of fewer than 10 seconds can signal dry eye disease.
Healthcare providers also may order other tests, such as antibody tests, to check for underlying conditions that could be causing your dry eye.
How can I reduce my risk of dry eye?
Dry eye disease has many causes, so it can be hard to prevent. You may be able to reduce your risk by:
- Visiting a healthcare provider for yearly checkups. A primary care physician can help you with your overall health. If you’re concerned about developing dry eye, talk to your provider. Ask if anything in your medical history or medications list puts you at risk. And ask what you can do to lower that risk.
- Managing underlying conditions. Many different conditions, including diabetes, can lead to dry eye. Talk to your healthcare provider about your risk for diabetes, and follow their advice for managing your blood sugar levels.
- Making lifestyle and environment changes. There’s a lot you can do in your daily life to lower your risk of dry eye. If you use a computer daily, take frequent breaks. Avoid cigarette smoke. Add a humidifier to your bedroom and other rooms where you spend a lot of time. Plus, ask a provider for other suggestions to help keep your eyes lubricated and healthy.
How to Treatment dry eye or eye dryness?
For most people with occasional or mild dry eye symptoms, it’s enough to regularly use nonprescription eye drops, also called artificial tears. If your symptoms are persistent and more serious, you have other options. What you do depends on what’s causing your dry eyes.
Some treatments focus on reversing or managing a condition or factor that’s causing your dry eyes. Other treatments can improve your tear quality or stop your tears from quickly draining away from your eyes.

Punctal plugs
One approach to treating dry eyes is plugging the openings to the tear ducts with tiny silicone plugs (punctal plugs). These plugs close the tiny opening (punctum) that you have in the inner corner of your upper and lower eyelids. The closure conserves both your own tears and artificial tears you may have added.
Treating the underlying cause of dry eyes
In some cases, treating an underlying health issue can help clear up the signs and symptoms of dry eyes. For instance, if a medication is causing your dry eyes, your eye care specialist may recommend a different medicine that doesn’t cause that side effect.
If you have an eyelid condition, such as your lids turned outwards (ectropion), your eye care specialist may refer you to an eye surgeon who specializes in plastic surgery of the eyelids (oculoplastic surgeon).
Medications
Prescription medicines used to treat dry eyes include:
- Medicines to reduce eyelid inflammation. Inflammation along the edge of your eyelids can keep oil glands from secreting oil into your tears. Your eye care specialist may recommend antibiotics to reduce inflammation. Antibiotics for dry eyes are usually taken by mouth, though some are used as eye drops or ointments.
- Eye drops to control cornea inflammation. Inflammation on the surface of your eyes (cornea) may be controlled with prescription eye drops that contain the immune-suppressing medicine cyclosporine (Restasis) or corticosteroids. Corticosteroids are not ideal for long-term use due to possible side effects.
- Eye inserts that work like artificial tears. If you have moderate to severe dry eye symptoms and artificial tears don’t help, another option may be a tiny eye insert that looks like a clear grain of rice. Once a day, you place the hydroxypropyl cellulose (Lacrisert) insert between your lower eyelid and your eyeball. The insert dissolves slowly, releasing a substance that’s used in eye drops to lubricate your eye.
- Tear-stimulating medicines. Medicines called cholinergics (pilocarpine, cevimeline) help increase tear production. These medicines are available as pills, gels or eye drops. Possible side effects include sweating.
- Eye drops made from your own blood. These are called autologous blood serum drops. They may be an option if you have severe dry eye symptoms that don’t respond to any other treatment. To make these eye drops, a sample of your blood is processed to remove the red blood cells and then mixed with a salt solution.
- A nasal spray to increase tear production. The Food and Drug Administration (FDA) recently approved varenicline (Tyrvaya) to treat dry eyes. This medicine is delivered via a nasal spray. Varenicline is to be sprayed once into each nostril, twice a day.
Other procedures
Other procedures that may be used to treat dry eyes include:
- Closing your tear ducts to reduce tear loss. Your eye care specialist may suggest this treatment to keep your tears from leaving your eye too quickly. This can be done by partially or completely closing your tear ducts, which normally serve to drain tears away.
Tear ducts can be plugged with tiny silicone plugs (punctal plugs). These are removable. Or tear ducts can be plugged with a procedure that uses heat. This is a more permanent solution called thermal cautery.
- Using special contact lenses. Ask your eye care specialist about newer contact lenses designed to help people with dry eyes.
Some people with severe dry eyes may opt for special contact lenses that protect the surface of the eyes and trap moisture. These are called scleral lenses or bandage lenses.
- Unblocking oil glands. Warm compresses or eye masks used daily can help clear up blocked oil glands. A thermal pulsation device is another way to unclog the oil glands, but it is unclear whether this method provides any advantage over warm compresses.
- Using light therapy and eyelid massage. A technique called intense-pulsed light therapy followed by massage of the eyelids may help people with severe dry eyes.
Does dry eye go away?
Dry eye is a chronic condition. It doesn’t have a cure, but treatments can help manage your symptoms.
You may have to try several different treatments to find what works best for you. This can be a stressful process, but it’s worth the effort. Talk to your provider if your current treatments aren’t working or you want to discuss other options.
How do I take care of myself with dry eye?
Living with dry eye isn’t easy. Many people experience stress, anxiety and exhaustion from trying to manage symptoms. If your condition affects your quality of life, talk to your healthcare provider. You may need to try many different treatments before finding an approach that manages your symptoms.
Keep in mind that millions of people have dry eye. So, you don’t have to deal with it alone. Connect with support communities online, and ask your provider for suggestions. Sharing your challenges with others who understand what you’re going through can be a huge help in your day-to-day life.
When should I see my healthcare provider?
Your ophthalmologist will tell you how often you need to come in for appointments. If other medical conditions are causing your dry eye, you may need regular follow-ups with other healthcare providers, too. Be sure to go to all of your appointments so your care team can monitor your condition and help you receive treatment.
Call your ophthalmologist if you experience:
- New symptoms.
- Symptoms that get worse.
- New side effects from treatments.
What is epiphora?
Epiphora is the medical term for having watery eyes.
Usually, tears lubricate and protect your eyes. Epiphora happens when something causes you to make too many tears or stops them from draining away from your eyes like they should.
Epiphora can happen for lots of reasons, many of which don’t need any treatment. It can be a temporary condition, but it can also be a sign of a serious eye infection or a blockage in your tear ducts. Visit your healthcare provider if your eyes are constantly watering or you’re having trouble seeing.
Who does epiphora affect?
Anyone can be affected by epiphora. Most people experience watery eyes at some point throughout their life.
Epiphora that happens frequently — chronic watery eyes — is more common in babies and adults older than 50.
How does epiphora affect my body?
Having watery eyes is the most obvious way epiphora will affect you. Having one watery eye is sometimes referred to as unilateral epiphora. If both your eyes are watery at the same time you have bilateral epiphora.
Depending on what’s causing the epiphora, you might also experience other issues in or around your eyes, including:
- Eye pain.
- Itchiness.
- Red eye.
- Cloudy or unclear vision.
- Sinus headaches.
What are the symptoms of watery eyes?
Symptoms of epiphora include:
- Eyes that feel too wet or watery.
- Tears running down your face.
- Tears building up in your eyes when you’re not crying or laughing.
What causes watery eyes?
Watery eyes are usually a sign of another issue or condition that’s affecting your eyes or tear system. Some of the most common causes of epiphora include:
- Allergies.
- Blepharitis.
- Blocked tear ducts (nasolacrimal duct obstruction).
- Dry eyes.
- Styes.
- Chalazions.
- Entropion.
Eye injuries can also cause epiphora, including:
- Environmental irritants like smoke or air pollution.
- Scratched corneas (corneal abrasions).
- Dirt, debris, chemicals or any foreign object that touches your eye for too long.
Infections like pink eye (conjunctivitis) or sinus infections (sinusitis) can cause watery eyes, as well.
How is epiphora diagnosed?
Your healthcare provider or eye care specialist will diagnose epiphora with an eye exam. They might put colored eye drops in your eyes to see how they drain. Usually, your tears will wash the drops and dye away from your eye in a few minutes. If they don’t, there’s a chance you have a blocked tear duct. You might need a few imaging tests, including:
- X-rays.
- CT scan.
Your provider might use an endoscope — a long, flexible tube with a light on the end — to look inside your nasal cavity if they think the epiphora is caused by an issue in your tear ducts or sinuses.
How is epiphora treated?
How your watery eyes are treated depends on what’s causing them? Many people experience temporary epiphora that clears up on its own without any treatment.
Your provider will tell you which type of treatment you’ll need. The most common treatments include:
- Medications: You’ll need medication to treat your watery eyes if the epiphora is caused by allergies or an infection. If you have a condition like dry eye syndrome, your provider might prescribe artificial tears or prescription eye drops.
- Removing foreign objects: If there’s something in your eye or something hit your eye and damaged it, your provider will remove it or treat the damage. You might need surgery if a foreign object severely damaged your eye.
- Clearing blocked tear ducts: If you have blocked tear ducts, your provider will open them. They can flush them with a saline solution to rinse away the blockage. They can use a probe to open your tear ducts manually if they need to. If your tear ducts are damaged or blocked by something your provider can’t remove with either saline or a probe, you might need surgery to open them.
- Repairing your eyes or eyelids: If the physical shape of your eyes or eyelids is causing epiphora, your provider will repair the damage. You might need surgery to correct some issues.
How do I manage symptoms of watery eyes?
Your eye doctor will tell you how to manage your epiphora symptoms. If they prescribe a medication, make sure to take it or use it as often as they say.
This is especially true if they give you antibiotics for an infection. You need to take antibiotics for as long as your provider prescribes, even if your symptoms improve. If you don’t take the full course of antibiotics, the infection might come back, get worse or spread to other parts of your body.
Don’t rub your eyes. Don’t touch your eyeball with anything like a tissue or towel if you’re using one to dry excess tears — you might damage your eye or aggravate the cause of your watery eyes.
How can I reduce my risk of epiphora?
Depending on what’s causing your watery eyes, there might not be any way to prevent them. If your eyes are irritated by something in the air, or you’re experiencing allergy symptoms, you probably can’t avoid watery eyes.
Make sure to wear all the proper equipment — including eye protection or goggles — for any work or activity that might hurt your eyes.
If you can, avoid your allergy triggers.
Talk to your eye doctor about ways you might be able to prevent watery eyes in the future.
What can I expect if I have epiphora?
Most cases of epiphora are temporary. Your eyes might only be watery during allergy season, or until your eye heals after being irritated by a foreign object. But — even if you need treatment — you should expect your watery eyes to get better. Talk to your provider about what to expect based on what’s causing your watery eyes.
Will I need to miss work or school while I’m recovering from epiphora?
You probably won’t need to miss work or school while you’re recovering from epiphora. You might have to take time off your job or miss some classes if you need surgery to repair damage to your eye, or if your watery eyes are affecting your vision.
Talk to your provider or surgeon before resuming any physical activities after surgery
When should I see my ophthalmologist?
Visit your doctor if you have any of the following symptoms:
- Eye pain.
- Swelling.
- You feel or see a lump or bump in your eye.
- Your eyes are watery all the time.
- You notice any changes in your vision or watery eyes make it hard to see clearly.
Go to the emergency room if you’ve experienced trauma or you suddenly lose vision in one or both of your eyes.
What questions should I ask my doctor?
- What’s causing my watery eyes?
- Which tests will I need?
- Will I need any treatment?
- How long should I take medication?
- What can I do to prevent epiphora in the future?
What is the difference between epiphora and lacrimation?
Lacrimation is the healthy production of tears in your eyes that happens automatically. Tears lubricate and protect your eyes.
You have two sets of lacrimal glands that make up your tear system. Your main lacrimal glands near the upper outer corner of each of your eyes produce tears to flush foreign materials out of your eyes. They also make tears when you’re crying. Your accessory lacrimal glands are behind your upper and lower eyelids. They produce the tears that moisten your eyes.
Epiphora is the medical definition for having excess tears or watery eyes. It’s caused by your eyes producing too many tears, or the tears in your eyes not draining away as they should.
What is a blocked tear duct?
The tears that moisturize your eye drain through a tiny opening in the corner of your eye. The liquid enters your nose, where your body absorbs and disposes of it.
A blocked tear duct is a full or partial obstruction (blockage) in the nasal (nose) passageways that drain tears. If you have a blocked tear duct, your eyes may be itchy, irritated and watery. Another name for a blocked tear duct is nasolacrimal duct obstruction. Lacrimal refers to tears.
How does the tear system work?
Typically, your tear system keeps your eyes slightly wet but not too watery. Your tear system has three parts:
- Lacrimal glands create tears.
- Puncta are small openings at your eye corner where tears flow out.
- Nasolacrimal ducts connect to the puncta and drain the rest of your tear fluid into the nose.
What are the tear ducts?
Tear ducts are another name for the nasolacrimal ducts. They form at the corner of your eye nearest your nose. They run underneath the skin and connect to your facial bones and nose.
How does a clogged tear duct affect my body?
When you have a clogged tear duct, tears can’t drain into the nose through the nasolacrimal ducts. Instead, your tears stay in your eye. The result is uncomfortable, watery eyes.
What is a partial tear duct blockage?
Sometimes, a narrow tear duct (dacryostenosis) can lead to a partial tear duct blockage. When you have a partial blockage, your tears may build up and not drain properly. This tear buildup can lead to infection. If you have a partial blockage, your provider will likely use similar treatments as a full blockage.
Who might get a blocked tear duct?
Blocked tear ducts are common in newborns. Usually, a blocked tear duct in a baby goes away without treatment.
Adults are more likely to develop a tear duct blockage if they have:
- Chronic eye inflammation, such as uveitis.
- Glaucoma.
- History of eye or sinus surgery.
- Previous cancer treatment, such as radiation therapy or chemotherapy.
What causes a blocked tear duct?
Blocked tear ducts can happen to anyone of any age. Causes of blocked tear ducts include:
- Age: As you get older, your puncta may naturally narrow.
- Congenital blockages: Some babies are born with tear ducts that are narrow or not fully formed (dacryostenosis).
- Infection: Chronic sinus infections or eye infections can lead to blockage.
- Injury: Any eye injury near the tear ducts, even a scrape from tiny dirt particles, can cause a blockage.
- Tumors: A tumor anywhere near the tear ducts, such as in the nose, can cause blocked tear ducts.
What are the symptoms of a blocked tear duct in adults?
The most common sign of a blocked tear duct is watery eyes or excessive tearing. You may also experience:
- Blurred vision.
- Crusting around the eyelids.
- Drainage, such as mucus or pus around the eyes.
- Redness in the white part of your eye.
- Swelling near your eye’s inner corner.
What are the symptoms of a blocked tear duct in infants?
Babies don’t start making tears until they are a few weeks old. You may not notice a blocked tear duct in a newborn right away. As babies get older, blocked tear duct symptoms might include:
- Redness around the eye, usually from your baby rubbing the eye.
- Tears draining down the baby’s cheek instead of out of the eye corner.
- Tears pooling near the corner of the eye but not draining.
- Yellowish discharge or mucus in the baby’s eye.
What tests can help diagnose a blocked tear duct?
To diagnose a blocked tear duct, your healthcare provider asks about your symptoms. Your provider may also use tests that examine the eyes and nose, including:
- Tear drainage test: Your provider places one drop of dye on each eye. If the dye does not drain from your eye, it could mean you have a blocked tear duct.
- Eye imaging: Your provider puts a special, safe dye in your eye. This dye travels through your tear drainage system. It shows up on an X-ray, CT scan or MRI to help your provider find the blockage.
- Irrigation and probing: Irrigation uses a fluid to clean out your tear ducts. Your provider may insert a small instrument through the corner of your eye to find the obstruction.
What is the treatment for a blocked tear duct in adults?
Blocked tear duct treatment depends on the cause. For example, if you have a tumor, your treatment focuses on removing or shrinking the tumor.
Additional treatment options may include:
- Medications: If an eye infection caused the blockage, your provider may prescribe oral antibiotics or medicated eyedrops.
- Dilation, probing and flushing: Your provider enlarges the opening at the corner of your eye. Then, using a small probe, your provider sends fluid through the tear duct. Usually, this “flushing” removes the blockage at least temporarily.
- Stenting: Your provider places a small, hollow tube (stent) through the puncta and into the tear duct. The tube allows tears to drain properly. The tubes stay in place for about three months. You will see a small portion of the tube out of the corner of your eye.
- Balloon catheter dilation: Your provider places a small, deflated balloon into the tear duct. Then your provider inflates the balloon a few times to clear the blockage. You are usually under general anesthesia (medication to help you remain asleep) for this procedure.
- Snip punctoplasty: Your provider makes two or three small incisions around your puncta. These incisions create a larger tear duct opening. Snip punctoplasty is a common treatment for partial blockages.
What is dacryocystorhinostomy for blocked tear ducts?
If less-invasive options don’t bring relief, your provider may recommend surgery. Providers usually use dacryocystorhinostomy (DCR). This procedure creates a new route to drain tears into your nose.
On the day of surgery, you receive anesthesia to help you stay calm and numb during the operation. During the procedure, your surgeon:
- Creates a connection between your lacrimal sac and nose. The surgeon may use small incisions or place tools through the nose.
- Places stents (small, hollow tubes) to hold open the new route as it heals.
A dacryocystorhinostomy is usually an outpatient surgery, meaning you can go home the same day. Typically, your surgeon removes the stents after three to four months.
What is the treatment for a blocked tear duct in babies?
Often, a blocked tear duct in a newborn resolve without treatment. In the first few months of life, the baby’s tear ducts may mature and get rid of the blockage.
Sometimes, a baby still has a small piece of tissue blocking the flow of tears inside the nose. Your baby’s provider may teach you a special eyelid massage technique. This massage helps open the tissue so tears can drain as they should.
If a watch-and-wait approach does not work, providers may use dilation and flushing, balloon catheters or stents. These treatments work the same way in babies as they do in adults. However, providers use general anesthesia to keep babies still and calm during the procedure.
How can I prevent a blocked tear duct?
The best way to avoid a blocked tear duct is to get care right away for eye problems, such as inflammation, infection or injury. To prevent eye inflammation or infections:
- Avoid rubbing or excessively touching your eyes.
- Avoid sharing eye products, such as eyedrops or cosmetics.
- Clean contact lenses according to your eye doctor’s instructions.
- Replace cosmetics, such as mascara, eyeliner or eyeshadow, every three to six months.
- Wash your hands frequently and thoroughly.
What is the outlook for blocked tear ducts?
If the blocked tear duct is because of an injury, it usually clears up on its own once the injury heals. Blocked tear ducts in babies often open up in time or with home care.
People who receive blocked tear duct treatment typically have an excellent outlook. In particular, dacryocystorhinostomy has around a 90% success rate. Most people don’t have any further symptoms after treatment.
What else should I ask my healthcare provider?
You may also want to ask your healthcare provider:
- What is the most likely cause of a blocked tear duct?
- What treatments do you recommend?
- Are there any treatment side effects?
- Is the tear duct blockage related to another medical condition?
- How can I prevent the blockage from returning?
Why is an Oculoplasty Procedure performed?
An Oculoplasty is typically performed for the following reasons:
- Congenital: Oculoplasty surgery can be conducted for congenital deformities, including gaps in the eyelids, abnormal position of eyelids, abnormal shape and size of orbits, blocked tear drainage passages, etc.
- Traumatic (Injury): Oculoplasty surgeries can be conducted to repair eyelid injuries, scar development, orbito-facial fractures,loss of eyeball, etc. The surgery can result inbetter eye functioning and look.
- Age-related: The operation can be conducted for troublesin-turning or out-turning of the eyelids and rubbing of eye-lashes on the eye, droopy and lax eyelids, eyelid bags, herniation of orbital fats etc. Oculoplasty operations can efficiently correct these difficulties.
- Tumour: Tumours and cancers of the lids and orbits are managed by oculoplastic surgeries. These procedures can save life and vision.
- Blocked tear ducts: Blocked tear ducts will cause watering of eyes with discharge. This can also cause repeated infections of the eyes and the surrounding areas of the face leading to serious damage to life and vision. DCR or Dacryocystorhinostomy and DCT or Dacryocystectomy are the procedures we perform for the blocked tear ducts.
- Thyroid Eye Disease: Thyroid diseases can cause serious problems of eye lids and orbits amongst other things. If medicines do not work then oculoplastic surgeries are necessary to manage the conditions.
What is the Treatment of Oculoplasty
The oculoplasty treatment starts with a detailed eye examination to understand the current state of the patient’s eye condition. This will help the ophthalmologist have a deeper understanding of the difficulties the patients face in their vision. Once this test is done, the patients are advised to undergo the appropriate oculoplastic procedures to cure their condition.
The patients will be free to pick any of them. Once they have decided to proceed with the procedure, we will give them full support with the latest tools, advanced technology, and well experienced oculoplastic surgeons so that the surgery becomes easy for them.
What does oculoplastic mean?
Oculoplastics, or oculoplastic surgery, describes a set of surgical procedures on the eye and its surrounding structures, including the eyelids, tear ducts, eye sockets, and parts of the face.
Oculoplasty, or ophthalmic plastic surgery, is performed to improve the function and comfort of the eye. It can also treat tear drainage problems, eyelid malposition, issues with the eye socket or eyebrows, and skin cancers of the eyelid.
Brow Lift FAQ: What You Need To Know
Browlift, Eyelid surgery, Facelift, Forehead Lift, Upper eyelid surgery
Eyebrow Lift surgery is a procedure designed to dramatically erase the horizontal wrinkles in the forehead that cause eyebrows to sag. This helps to produce a more youthful, fresher appearance that can restore confidence.
If you’re considering a brow lift, take a look at these commonly asked questions from prospective patients.
What does a brow lift involve?
Traditional methods for this procedure required a large incision site along the hairline that lengthened recovery time. Now thanks to advancements in technology, only 3-5 very small incisions along the hairline are needed to perform this procedure. Smaller incisions require less recovery time and produce minimal scarring.
Who is a good candidate for brow lift?
The best candidates are those who have deep horizontal wrinkles in their forehead or between the eyes, or sagging eyebrows. Wrinkles in the forehead and droopy eyebrows tend to make people look older, sad, and tired, and this procedure helps patients to look as young as they feel!
What can I expect during recovery?
Generally, this procedure is performed on an out-patient basis and results are noticeable immediately. However, after surgery it is common to be swollen for the first few weeks. Results will increase over time, usually within a 6 month period. Scars will also fade over time.
What are the risks associated with brow lifts?
Serious risks and complications are rare with this procedure, however, any surgery involves some level of risk. Some patients suffer adverse reactions to anesthesia, or injury to facial tissue.
What type of results can I expect?
Results of a brow lift procedure can be subtle or dramatic. Your individual results will be determined by the surgical goals expressed during your consultation.
What is a brow lift?
A brow lift is a surgical procedure that is performed to return the brow back to its natural, refreshed position. We tend to get horizontal wrinkles across our forehead-why? Because we all tend to raise our brows in order to reduce the fold above our eyes that can begin to affect our peripheral vision (and, let’s be honest, raising our brow makes us look better in a selfie). A brow lift relieves this tension by raising the brow-so you don’t constantly flex your forehead muscles that can give you a chronic headache or strain.
What is the difference between blepharoplasty and a brow lift?
A Blepharoplasty reduces the fold above the eye by reducing fat pockets and excess skin. The fat pockets come forward as the skin loses elasticity and ages. A brow lift raises the brow to further reduce the fold above the eyes. Our brows fall due to an involuntary muscle pull that often creates the “11’s” between the brows, as well as genetic factors and gravity pulling the brow down.
Is a brow lift (forehead lift) better to raise sagging eyelids than a blepharoplasty?
One procedure is not better than the other, rather, they compliment each other. We see a lot of patients who wish for the entire fold above the eye to be gone with a blepharoplasty (reducing the skin above and eye) but here is what most people do not understand- 50% of the fold often is caused by a low brow position. If the brow is not raised, and the entire fold is removed, this would make the brows even lower! Often, combining a brow lift with a blepharoplasty can optimally reduce the lid fold with a natural refreshed look because it keeps your face in it’s natural proportions.
Can asymmetric eyes or eyebrows be fixed?
Most of us have some level of asymmetry in our facial anatomy. Surgery may help balance some level of brow asymmetry (and Botox can also play a key role in balancing the brows as well!)
Will I have visible scars after surgery?
What can I do to lessen scars? The incisions that are created for the brow lift are hidden in the hairline. Depending on the thickness of the hair in the area will determine visibility.
What is recovery from brow lift like?
You may have some bruising and swelling after surgery that will resolve in several days as you ice the area
What is Blepharoplasty?
Blepharoplasty (BLEF-uh-roe-plas-tee) is a type of surgery that removes excess skin from the eyelids. With age, eyelids stretch, and the muscles supporting them weaken. As a result, excess skin and fat can gather above and below your eyelids. This can cause sagging eyebrows, droopy upper lids and bags under the eyes.
Besides aging, severely sagging skin around the eyes can reduce side vision (peripheral vision), especially the upper and outer parts of the visual field. Blepharoplasty can reduce or get rid of these vision problems. The surgery can also make eyes look younger and more alert.
What happens in a blepharoplasty?
A blepharoplasty is a surgical rejuvenating procedure that may be performed on the upper and/or lower eyelids. An upper blepharoplasty may include excision of drooping eyelid skin, repair of the muscle that opens the eyes, and removal of excess fat.
How do you know if you need blepharoplasty?
If you have droopy or sagging eyelids that keep your eyes from opening completely and interferes with your peripheral vision,you might need a blepharoplasty. This procedure removes excess tissue from your eyelids and thereby improves your vision.
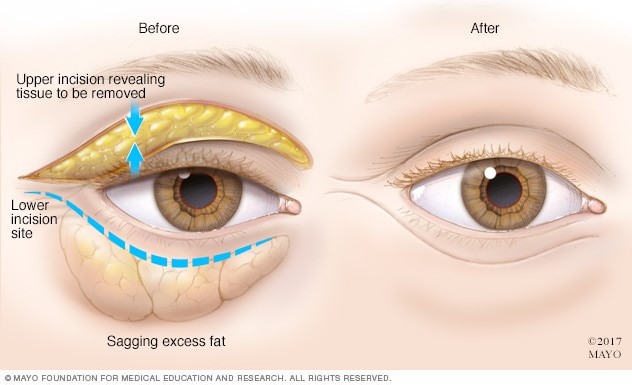
Why it’s done?
Blepharoplasty might be an option for:
- Baggy or droopy upper eyelids
- Excess skin of the upper eyelids that partially blocks peripheral vision
- Excess skin on the lower eyelids
- Bags under the eyes
Blepharoplasty can be done at the same time as another procedure, such as a brow lift, face-lift or skin resurfacing.
What is the Risks of surgery?
All surgery has risks, including reaction to anesthesia and blood clots. Besides those, rare risks of eyelid surgery include:
- Infection and bleeding
- Dry, irritated eyes
- Difficulty closing the eyes or other eyelid problems
- Noticeable scarring
- Injury to eye muscles
- Skin discoloration
- Temporarily blurred vision or, rarely, loss of eyesight
- The need for follow-up surgery
How you prepare?
Before scheduling blepharoplasty, you’ll meet with oculoplastic surgeon. Providers you meet with may include a plastic surgeon, an eye specialist (ophthalmologist), or an ophthalmologist who specializes in plastic surgery around the eyes (oculoplastic surgeon). The discussion includes:
- Your medical history. Your care provider will ask about previous surgeries. Your provider may also ask about past or current conditions such as dry eyes, glaucoma, allergies, circulatory problems, thyroid problems and diabetes. Your provider will also ask about your use of drugs, vitamins, herbal supplements, alcohol, tobacco and illegal drugs.
- Your goals. A discussion of what you want from the surgery will help set the stage for a good outcome. Your care provider will discuss with you whether the procedure is likely to work well for you.
Before your eyelid surgery, you’ll likely have a physical exam and the following:
- Complete eye exam. This might include testing tear production and measuring parts of the eyelids.
- Visual field testing. This is to see if there are blind spots in the corners of the eyes (peripheral vision). This is needed to support an insurance claim.
- Eyelid photography. Photos from different angles help with planning the surgery, and documenting whether there’s a medical reason for it, which might support an insurance claim.
And your provider will likely ask you to do the following:
- Stop taking warfarin (Jantoven), aspirin, ibuprofen (Advil, Motrin IB, others), naproxen sodium (Aleve, others), naproxen (Naprosyn), and other drugs or herbal supplements that can increase bleeding. Ask your health care provider how long before surgery to stop taking these drugs. Take only drugs approved by your surgeon.
- Quit smoking several weeks before surgery. Smoking can reduce the ability to heal after surgery.
- Arrange for someone to drive you to and from surgery if you are having outpatient surgery. Plan to have someone stay with you for the first night after returning home from surgery.
What you can expect?
Before the procedure
Blepharoplasty is usually done in an outpatient setting. You might be given drugs such as injections into the eyelids to numb them and drugs through an IV to help you relax.
During the procedure
For upper eyelids, the surgeon cuts along the fold of the eyelid. The surgeon removes some excess skin, muscle and possibly fat. Then the surgeon closes the cut.
On the lower lid, the surgeon makes a cut just below the lashes in your eye’s natural crease or inside the lower lid. The surgeon removes or redistributes excess fat, muscle and sagging skin. Then the surgeon closes the cut.
If your upper eyelid droops close to your pupil, your surgeon may do blepharoplasty combined with a procedure called ptosis (TOE-sis). Ptosis is designed to lift the eyelid as well as remove excess eyelid skin.
After the procedure
After surgery you spend time in a recovery room where staff members monitor you for complications. You can leave later that day to heal at home.
After surgery you might temporarily have:
- Blurred vision from the lubricating ointment applied to your eyes
- Watering eyes
- Light sensitivity
- Double vision
- Puffy, numb eyelids
- Swelling and bruising similar to having black eyes
- Pain or discomfort
Take the following steps to help you recover from surgery unless your surgeon gives you different instructions.
Do:
- Use ice packs on your eyes for 10 minutes every hour the night after surgery. The following day, use ice packs on your eyes 4 to 5 times throughout the day.
- Use prescribed eye drops or ointments.
- Sleep with your head raised higher than your chest for a few days.
- Apply cool compresses to reduce swelling.
- Wear dark sunglasses to protect the skin of your eyelids from sun and wind.
- If needed, use acetaminophen (Tylenol, others) to control pain.
Don’t:
- Do anything strenuous for a week — no heavy lifting, swimming, jogging or aerobics.
- Smoke.
- Rub your eyes.
- Wear contact lenses for about two weeks.
- Take aspirin, ibuprofen (Advil, Motrin IB, others), naproxen sodium (Aleve, others), naproxen (Naprosyn), and other drugs or herbal supplements that can increase bleeding.
As instructed, return to the care provider’s office to have stitches removed, if needed.
Seek medical attention immediately if you have any of the following symptoms:
- Shortness of breath
- Chest pain
- An unusual heart rate
- Severe new eye pain
- Bleeding
- Vision problems
What is the expected Results?
Many people who have blepharoplasty say they feel more self-confident and feel they look younger and more rested. For some people, surgery results may last a lifetime. For others, droopy eyelids can recur.
Bruising and swelling generally lessen slowly in about 10 to 14 days. Scars from the surgical cuts may take months to fade. Take care to protect your delicate eyelid skin from sun exposure.
What is Ptosis and does it affect vision?
Ptosis is a condition when the eyelid drops down and covers part of the eye. If the eyelid drops far enough to cover some of the pupil then it may affect the peripheral vision. Ptosis can be present at birth or it can develop later in life. If the ptosis is severe in young children it can affect the development of normal vision. In adults ptosis can block vision and be bothersome while reading or driving. Adults and children often try to compensate for the droopy eyelid by using the forehead muscles to help lift the eyelid.

Who is a candidate for surgical repair of ptosis?
Most patients who present with ptosis are good candidates for repair. As long as the patient is well and the eyelid healthy then the ptosis can usually be surgically repaired. Patients with moderate to severe dry eye are not good candidates for surgical repair, because elevating the eyelid position can make dry eye symptoms worse.
When a patient comes to my office with ptosis, I will evaluate the eyes for any medical conditions that may be underlying and causing the ptosis. Patients with an underlying condition is not a candidate for surgical repair. These include:
- Tumor around or behind the eye.
- Diabetes.
- Horner syndrome.
- Myasthenia gravis.
- Stroke.
- Swelling in the eyelid, such as with a stye.
Who is the best doctor to repair ptosis?
Ptosis should always be repaired by an oculoplastic surgeon trained in this procedure. The eyelid anatomy is complex. Ptosis surgery requires years of training and expertise to perfect. It is important that your surgeon has many years of experience performing surgical ptosis repair.
What is Ectropion?

Ectropion (ek-TROH-pee-on) is a condition in which your eyelid turns outward. This leaves the inner eyelid surface exposed and prone to irritation.
Ectropion is more common in older adults, and it generally affects only the lower eyelid. In severe ectropion, the entire length of the eyelid is turned out. In less severe ectropion, only one segment of the eyelid sags away from the eye.
Artificial tears and lubricating ointments can help relieve symptoms of ectropion. But usually surgery is needed to fully correct the condition.
What is symptoms of Ectropion?
Normally when you blink, your eyelids distribute tears evenly across your eyes, keeping the surfaces of the eyes lubricated. These tears drain into small openings on the inner part of your eyelids (puncta).
If you have ectropion, your lower lid pulls away from your eye and tears don’t drain properly into the puncta. The resulting signs and symptoms can include:
- Watery eyes (excessive tearing). Without proper drainage, your tears may pool and constantly flow over your eyelids.
- Excessive dryness. Ectropion can cause your eyes to feel dry, gritty and sandy.
- Irritation. Stagnant tears or dryness can irritate your eyes, causing a burning sensation and redness in your eyelids and the whites of your eyes.
- Sensitivity to light. Stagnant tears or dry eyes can irritate the surface of the cornea, making you sensitive to light.
When to see a doctor
See your doctor if your eyes are constantly watering or irritated, or your eyelid seems to be sagging or drooping.
Seek immediate care if you have been diagnosed with ectropion and you experience:
- Rapidly increasing redness in your eyes
- Sensitivity to light
- Decreasing vision
These are signs and symptoms of cornea exposure or ulcers, which can harm your vision.
What Causes Ectropion?
Ectropion can be caused by:
- Muscle weakness. As you age, the muscles under your eyes tend to weaken, and tendons stretch out. These muscles and tendons hold your eyelid taut against your eye. When they weaken, your eyelid can begin to droop.
- Facial paralysis. Certain conditions, such as Bell’s palsy, and certain types of tumors can paralyze facial nerves and muscles. Facial paralysis that affects eyelid muscles can lead to ectropion.
- Scars or previous surgeries. Skin that has been damaged by burns or trauma, such as a dog bite, can affect the way that your eyelid rests against your eye. Previous eyelid surgery (blepharoplasty) can cause ectropion, particularly if a considerable amount of skin was removed from the eyelid at the time of surgery.
- Eyelid growths. Benign or cancerous growths on your eyelid can cause the lid to turn outward.
- Genetic disorders. Rarely is ectropion present at birth (congenital). When it is, it’s usually associated with genetic disorders, such as Down syndrome.
What is the Risk factors of ectropion?
Factors that increase your risk of developing ectropion include:
- Age. The most common cause of ectropion is weakening muscle tissue associated with aging.
- Previous eye surgeries. People who have had eyelid surgery are at higher risk of developing ectropion later.
- Previous cancer, burns or trauma. If you’ve had spots of skin cancer on your face, facial burns or trauma, you’re at higher risk of developing ectropion.
What is the Complications of Ectropion?
Ectropion leaves your cornea irritated and exposed, making it more susceptible to drying. The result can be abrasions and ulcers on the cornea, which can threaten your vision.
What is Ectropion Treatment
The treatment of the ectropion usually requires a day-case operation, typically taking 30-45 minutes under local anaesthetic. It is a very effective procedure, giving relief of symptoms with an excellent cosmetic outcome.
Surgery involves tightening of the lower lid, which can be achieved in different ways depending upon the severity of the ectropion and whether the whole or part of the eyelid is affected. Patients whose ectropion is caused by shortening of the skin of the eyelids may need a skin graft.
Following surgery, the eye is usually padded for at least a day to reduce swelling, and antibiotic drops or an ointment are prescribed. Stitches are removed 1-2 weeks later.
Ectropion Post-Operative Care?
- Check your vision daily by covering each eye and reading newspaper print.
- A pressure dressing may be applied for several days if your operation involves a skin flap or graft.
- Post-operative bruising and swelling may be minimized by applying a cold compress after surgery (10 minutes every 2 hours for 3 days), head elevation and Arnica tablets.
- Bathe the wounds gently using cool boiled water and a gauze wipe. Wash your hands thoroughly before and after bathing.
- An antibiotic ointment will be prescribed to apply to the skin wound and into the eye for 1 week after surgery. This will create a film across the front of the eye causing blurring of vision for about 30 minutes. Take care not to touch the eye with the nozzle of the tube.
What should I expect after surgery?
- Post-operative bruising and swelling always occurs after eyelid surgery and may last many weeks. Bruising often takes 3-4 weeks to resolve completely, and swelling a little longer. The final result is not seen for at least 3-4 months
- A ‘tight’ appearance to the eyelid, which may look ‘pulled’ upwards at the outer corner compared to the other side. This will settle and become more symmetrical as the swelling subsides and the tissues relax.
- Mild blurring of vision often occurs for a few weeks afterwards. It is usually helped by blinking.
- Some tearing and mucous discharge is to be expected for a few weeks after surgery.
- The skin wound may start to itch after a few days – this is a sign of wound healing.
- Numbness may occur around the area of the operation. This improves with time.
- Temporary dryness of the eyes may occur after surgery. Blink frequently in order to clear the tear film and keep the eye moist. A short course of lubricating eye drops or gel will be prescribed if necessary.
The wound is likely to feel uncomfortable for a couple of days. You may take simple analgesia such as paracetamol (aspirin, ibuprofen or other anti-inflammatory drugs should, ideally, be avoided).
Will my daily activities be affected?
- You can read, watch television and go outside immediately (wearing sunglasses if more comfortable)
- You should resume all medications on the day of surgery, except medicines which may increase the risk of post-operative bleeding. I will discuss this with you on the day of surgery.
- Drive when you feel safe and able to see properly.
- Avoid getting water directly into the wounds when showering or bathing to reduce the risk of infection.
- Do not rub your eye
- Avoid bending for 1 week
- Avoid heavy lifting for 2 weeks
- Avoid eye make-up for 3 weeks
- Avoid dusty environments for 1 week
- Avoid all strenuous activity for 3 weeks
- Avoid swimming for 4 weeks
Are there any risks?
Complications in the hands of a trained and experienced oculoplastic surgeon are very rare. However, risks include:
- Infection. This may be heralded by swelling and redness around the wound. Should this happen, you must contact your doctor.
- Asymmetry. Tightening of the lower eyelid on one side can give a ‘pulled up’ look to the operated eyelid but this settles as the tissues relax over time.
- Scarring. Initially, the incisions will appear red. However, the skin around the eyelids typically heals very well, such that after several weeks most wounds are almost invisible.
- Thickening of a skin graft (ectropion surgery only). This very unusual and, if it does occur, tends to settle after a few months.
What is an entropion and what are the symptoms?
An entropion refers to a condition in which the lower eyelid turns inwards against the surface of the eye.
A mild entropion causes irritation and watering of the eye. The irritation can lead to squeezing of the eyelids, which in itself causes further in-turning of the eyelid and more severe discomfort.

The eye may become red, and the cornea may become scratched by the eyelashes rubbing against it. Rarely, a severe infection of the cornea can occur, leading to potential permanent loss of vision.
Pending surgical correction, daily cleaning of the eyelids, and lubricant gel and ointment can help to relieve any irritation.
What causes an entropion?
The most common cause of a lower eyelid entropion is an age-related instability of the eyelid structures. The majority are, therefore, seen in older patients. Other causes include previous trauma, chemical injuries, and inflammation of the conjunctiva on the inside of the eyelid.
What is Entropion Treatment?
The management of entropion depends on it cause, but it frequently requires surgery to return the eyelid margin outwards to its correct position. The operation is typically very successful, giving relief of symptoms with an excellent cosmetic outcome.
Surgery involves stitches to evert the eyelid back to its normal position, which are often combined with a lid tightening procedure. Typically, it is a day-case operation, takes 30-45 minutes and is carried out under local anaesthesia.
The eye is usually padded afterwards for at least a day to reduce swelling, and antibiotic drops or an ointment are prescribed. The stitches are removed 1-2 weeks later.
Post-operative care is very similar to that described for ectropion surgery.
What should I expect after surgery?
- Post-operative bruising and swelling always occurs after eyelid surgery and may last many weeks. Bruising often takes 3-4 weeks to resolve completely, and swelling a little longer. The final result is not seen for at least 3-4 months
- A ‘tight’ appearance to the eyelid, which may look ‘pulled’ upwards at the outer corner compared to the other side. This will settle and become more symmetrical as the swelling subsides and the tissues relax.
- Mild blurring of vision often occurs for a few weeks afterwards. It is usually helped by blinking.
- Some tearing and mucous discharge is to be expected for a few weeks after surgery.
- The skin wound may start to itch after a few days – this is a sign of wound healing.
- Numbness may occur around the area of the operation. This improves with time.
- Temporary dryness of the eyes may occur after surgery. Blink frequently in order to clear the tear film and keep the eye moist. A short course of lubricating eye drops or gel will be prescribed if necessary.
- The wound is likely to feel uncomfortable for a couple of days. You may take simple analgesia such as paracetamol (aspirin, ibuprofen or other anti-inflammatory drugs should, ideally, be avoided).
Will my daily activities be affected?
- You can read, watch television and go outside immediately (wearing sunglasses if more comfortable)
- You should resume all medications on the day of surgery, except medicines which may increase the risk of post-operative bleeding. I will discuss this with you on the day of surgery.
- Drive when you feel safe and able to see properly.
- Avoid getting water directly into the wounds when showering or bathing to reduce the risk of infection.
- Do not rub your eye
- Avoid bending for 1 week
- Avoid heavy lifting for 2 weeks
- Avoid eye make-up for 3 weeks
- Avoid dusty environments for 1 week
- Avoid all strenuous activity for 3 weeks
- Avoid swimming for 4 weeks
Are there any risks?
Complications in the hands of a trained and experienced oculoplastic surgeon are very rare. However, risks include:
- Infection. This may be heralded by swelling and redness around the wound. Should this happen, you must contact your doctor.
- Asymmetry. Tightening of the lower eyelid on one side can give a ‘pulled up’ look to the operated eyelid but this settles as the tissues relax over time.
- Scarring. Initially, the incisions will appear red. However, the skin around the eyelids typically heals very well, such that after several weeks most wounds are almost invisible.
- Thickening of a skin graft (ectropion surgery only). This very unusual and, if it does occur, tends to settle after a few months.
Back To Home









